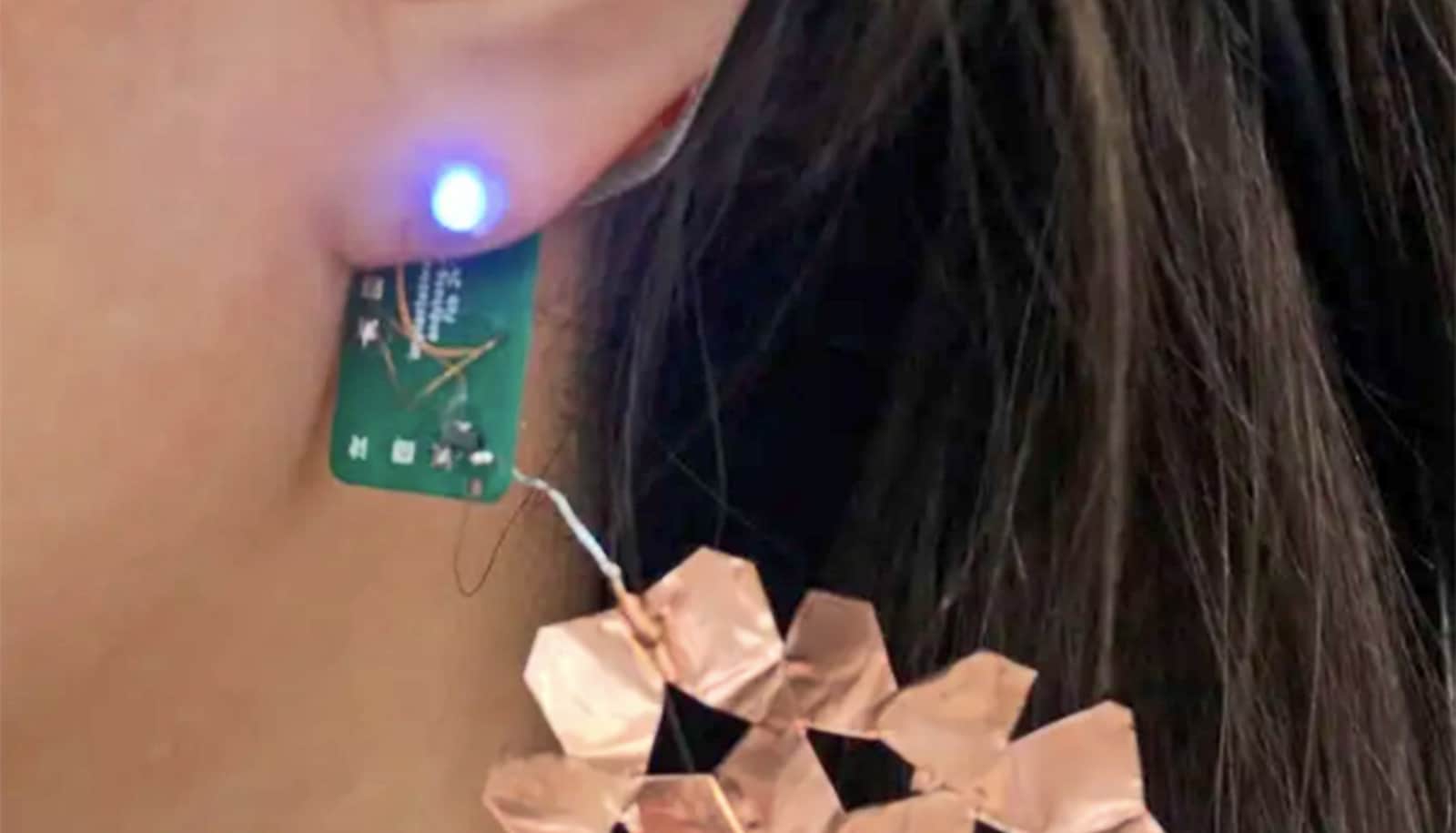
A stretchable wearable sensor designed to be worn on the throat can help monitor and treat stroke patients.
The sensor adds to the portfolio of stretchable electronics that are precise enough for use in advanced medical care and portable enough to be worn outside the hospital, even during extreme exercise, researchers say.
“Stretchable electronics allow us to see what is going on inside patients’ bodies at a level traditional wearables simply cannot achieve,” says John A. Rogers, engineering professor at Northwestern University. “The key is to make them as integrated as possible with the human body.”
The bandage-like throat sensor measures patients’ swallowing ability and patterns of speech and aid in the diagnosis and treatment of aphasia, a communication disorder associated with stroke.
The tools that speech-language pathologists have traditionally used to monitor patients’ speech function—such as microphones—can’t distinguish between patients’ voices and ambient noise.
“Our sensors solve that problem by measuring vibrations of the vocal cords,” Rogers says. “But they only work when worn directly on the throat, which is a very sensitive area of the skin. We developed novel materials for this sensor that bend and stretch with the body, minimizing discomfort to patients.”
Shirley Ryan AbilityLab, a research hospital in Chicago, uses the throat sensor in conjunction with electronic biosensors—also developed in Rogers’ lab—on the legs, arms, and chest to monitor stroke patients’ recovery progress.
“Talking with friends and family at home is a completely different dimension from what we do in therapy.”
The intermodal system of sensors streams data wirelessly to clinicians’ phones and computers, providing a quantitative, full-body picture of patients’ advanced physical and physiological responses in real time.
“One of the biggest problems we face with stroke patients is that their gains tend to drop off when they leave the hospital,” says Arun Jayaraman, research scientist at the Shirley Ryan AbilityLab and a wearable technology expert. “With the home monitoring enabled by these sensors, we can intervene at the right time, which could lead to better, faster recoveries for patients.”
Tiniest wearable sticks on your nail to monitor UV rays
Because the sensors are wireless, they eliminate barriers posed by traditional health monitoring devices in clinical settings. Patients can wear them even after they leave the hospital, allowing doctors to understand how their patients are functioning in the real world.
“Talking with friends and family at home is a completely different dimension from what we do in therapy,” says Leora Cherney, research scientist at the Shirley Ryan AbilityLab and an expert in aphasia treatment.
“Having a detailed understanding of patients’ communication habits outside of the clinic helps us develop better strategies with our patients to improve their speaking skills and speed up their recovery process.”
Robotic ‘exosuit’ fixes stride after stroke
The platform’s mobility is a “game changer” in rehabilitation outcomes measurement, Jayaraman says.
Data from the sensors will be presented in a dashboard that is easy for both clinicians and patients to understand. It will send alerts when patients are underperforming on a certain metric and allow them to set and track progress toward their goals.
The team presented their research last week at the American Association for the Advancement of Science (AAAS) annual meeting in Austin, Texas.
Source: Northwestern University