New findings clarify rare and puzzling cases of tuberculosis infecting the bones.
Tuberculosis is usually encountered as a disease of the lungs, but in 2% of cases in the US it can also be found in the bones. The 9,000-year-old skeletons of some Egyptian mummies show signs of having tuberculosis infection in their bones, a painful condition that leaves the bones looking like they’ve been gnawed.
So it was a weird puzzle when Duke physician Jason Stout encountered a Wake County, North Carolina TB outbreak in the mid-2000s in which the infection had spread beyond the lungs in six people. “Four out of six were in the bone,” Stout says. “That’s way more than 2%.”
The index case, the first person in Raleigh to have this strain of the disease, apparently contracted the bacterium in Vietnam, but he wasn’t feeling very sick and had been working around 400 people in his workplace.
“So it was prolonged exposure in a workplace,” says Stout, a Duke University professor of medicine who tracked down and identified seven subsequent infections through contact tracing and health department records.
All eight people were treated with antibiotics and other coworkers received preventative care and then the strange outbreak went away. But the mystery was never really solved. “I’m an epidemiologist and clinical trial specialist and I was left scratching my head,” Stout says.
Until several years later when Stout had a chance conversation with his colleague and TB researcher David Tobin, an associate professor in molecular genetics and microbiology and immunology at Duke.
“We met up and we’re having coffee one day, and we’re talking about this,” Stout recalls. Academic medical centers like Duke routinely keep biological specimens, and Stout still had samples of the puzzling bug. “David said, ‘Well, give it to me and we’ll take a look.’ And then this amazing science came from that,” Stout says.
The amazing science is that Tobin’s lab, with several colleagues at Duke, Notre Dame, and the University of Texas, figured out precisely how and why these particular TB bacteria were so mobile. Their findings appear in the journal Cell.
“Certain infections tend to go certain places,” Stout says. “And the question is always, why does it do that?” In TB strains found in the Americas and Europe, the bacteria seem more likely to stay put in the lungs. But this strain was highly mobile.
Tobin’s team ran genetic sequencing on the Raleigh bug and found it most resembled an ancestral strain from a group of strains called lineage 1. In the US we tend to see the modern strains, lineages 2, 3, and 4, but lineage 1 is still out there, mostly in South and Southeast Asia.
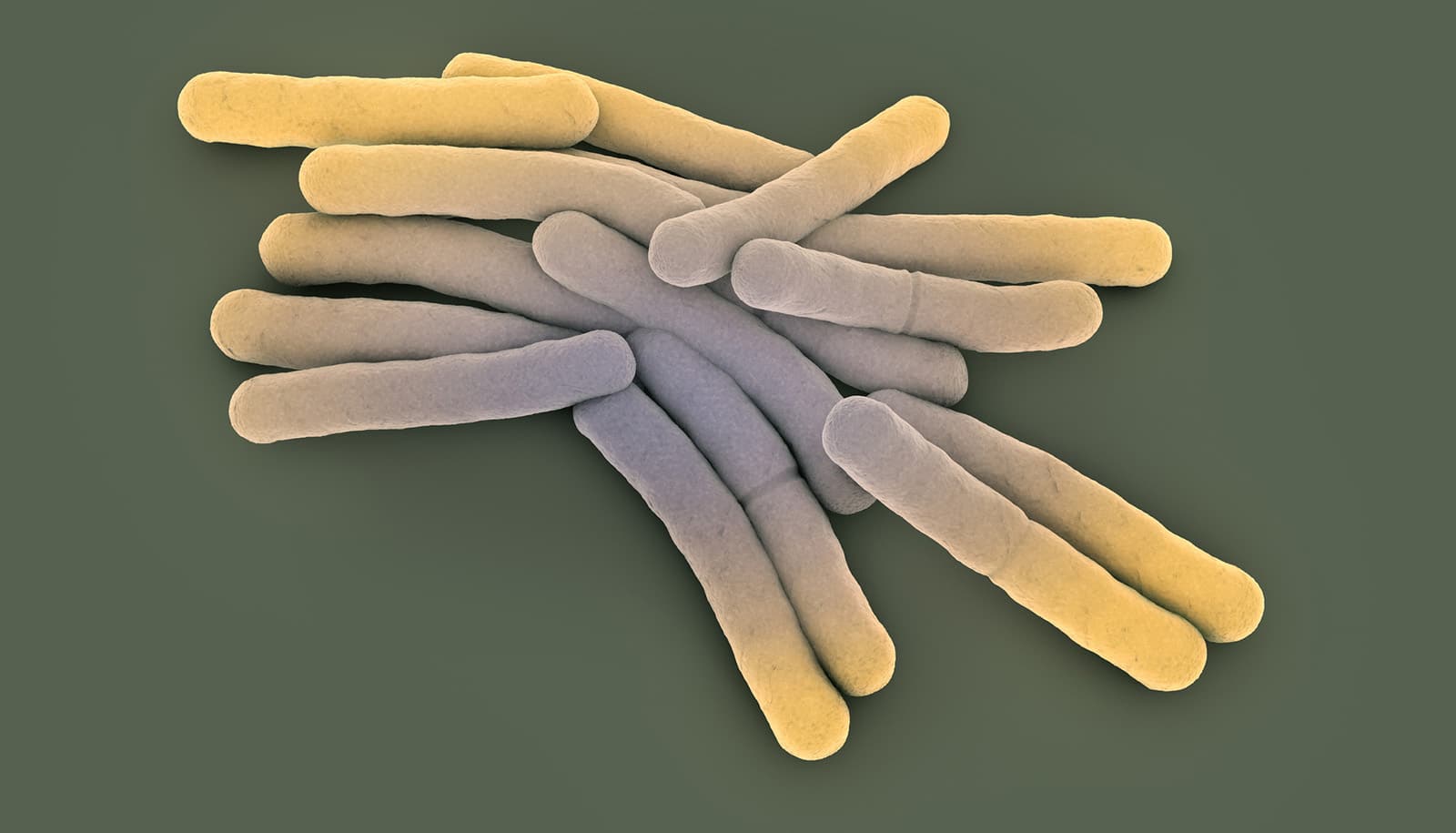
Mycobacterium tuberculosis generally infects a type of white blood cell called a macrophage, a highly mobile street sweeper cell that moves around looking for invaders and then engulfs them and chews them up. (Macrophage is Latin for big eater.) One part of the pathogenic bacteria’s toolkit is a set of unique chemical signals—secreted factors—to protect itself from the immune system and tell its macrophage host what to do.
Tobin’s team wanted to find the difference that allowed the Wake County bug’s macrophages to be more mobile and leave the lungs.
They compared genetic variants from 225 different strains of TB with particular attention to the genes for their secreted factors. What they found is a secretion factor called EsxM that was active in the Raleigh bacteria, but had been inactivated by a mutation in the modern strains.
Then, working with Craig Lowe, an evolutionary biologist and assistant professor of molecular genetics and microbiology at Duke, they looked at genetic sequencing from 3,236 different strains of TB and found the pattern persisted: the modern strains have a silenced version of the EsxM secretion factor. “Over a few thousand strains, that really holds up,” Tobin says. “They’ve maintained that and presumably it’s something that’s evolutionarily advantageous to them.”
To further prove their point, the researchers put active versions of EsxM into safely attenuated versions of modern strains and watched as their macrophage hosts in a lab dish became more active and mobile. “We can see these changes in macrophage shape and structure and they become more migratory,” Tobin says. They also knocked out EsxM in a strain with the ancestral version and made the infected macrophages less mobile.
While being careful not to overstate their findings, Tobin says it would appear that the broadly distributed modern strains of TB benefit from staying within the lungs because of the way they spread through the air by breathing. Staying in the lungs would presumably give them a better launching pad to a new host.
Fortunately, the migratory TB strain hasn’t been seen again locally, Stout says, “hopefully because we did good work and got a lot of people preventative therapy.” But the mystery of its strange mobility has been solved.
“This may well have ended with me saying, ‘Wow, that was weird. There’s got to be something about the strain because all these patients had healthy immune systems,'” Stout says. “But the kind of science that I do is not the kind of science that David does. This is a wonderful example of people from different disciplines coming together to answer a really interesting clinical problem.”
The National Institutes of Health supported the research.
Source: Duke University