New diagnostic tools such as machine learning and precision medicine could help identify tuberculosis patients with the highest risk of reactivation of the disease, report researchers.
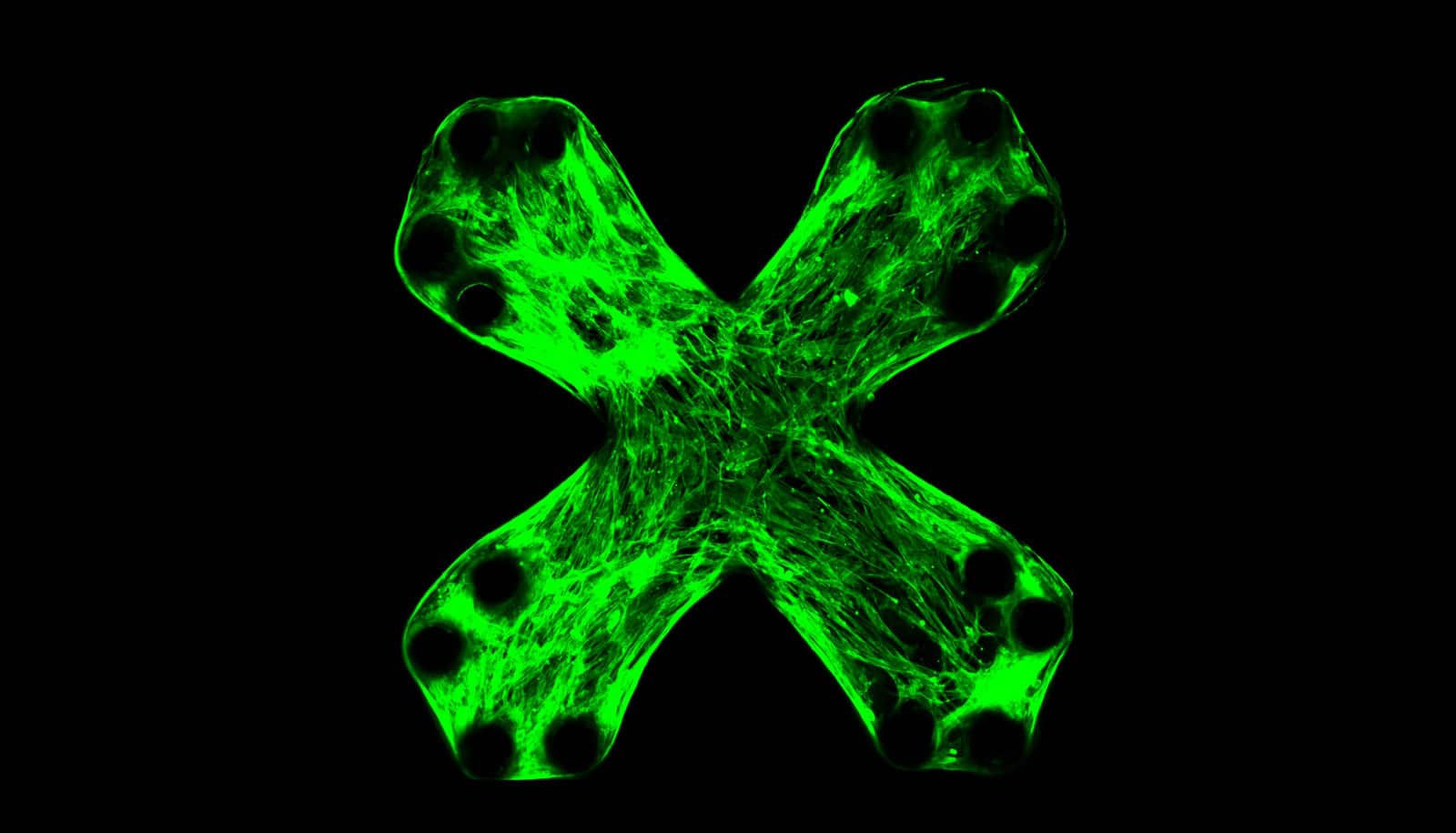
The researchers are showing that identifying multiple biomarkers can provide a more accurate diagnosis for patients.
“A multi-array test can provide a more detailed, disease specific glimpse into patient’s infection and likely outcome,” says Ryan Bailey, professor of chemistry at the University of Michigan and coauthor of the study, which appears in Integrative Biology.
“Using a precision medicine approach reveals previously obscured diagnostic signatures and reactivation risk potential.”
Latent tuberculosis infection (LTBI) affects nearly 2 billion people around the world and about 10 percent of those cases result in active tuberculosis. The reactivation from latency can happen anytime and the mechanism for it is not well-understood.
Currently, doctors test for LTBI using a skin scratch test or a blood test that identifies one biomarker but cannot distinguish between memory immune response, vaccine-initiated response, and non-tuberculous mycobacteria exposure. The possibility of correctly identifying the disease through these tests is less than 5 percent.
Doctors use an antibiotic regimen to treat tuberculosis, but that can increase the risk of antibiotic resistance.
The new diagnostic tools will help identify patients with the highest risk of reactivation and who will benefit from therapy, and reduce some of the side effects of overtreatment. By introducing multiple biomarker assays in blood tests with powerful analysis tools, the chances for correctly diagnosing TB increases dramatically.
The researchers used a precision normalization approach to correct for differences in individual basal immune function that revealed a high- and low-reactivation risk.
“This high-level multiplexing, high-assay performance can be cost-effective and scalable,” Bailey says, adding that it can also be used to detect other diseases like autoimmune diseases and cancer.
Additional researchers from the University of Michigan, the University of Illinois, and the Mayo Clinic in Rochester, Minnesota contributed to the study.
Source: University of Michigan