A “druggable” mechanism of tau protein pathology could lead to new treatment for some of the most devastating neurodegenerative diseases.
For the millions of people at risk for frontotemporal dementia and a host of other such conditions including Alzheimer’s disease, this could signal a shift toward significant management of symptoms or outright prevention of certain diseases.
“We’re super excited about this,” says Kenneth S. Kosik, professor of neuroscience at the University of California, Santa Barbara, and codirector of the university’s Neuroscience Research Institute.
While there is much more work to do, promising evidence for this treatable mechanism is mounting and setting the stage for future investigations. In the wake of the recent halting of clinical trials for Aducanumab, a drug that once looked like a promising Alzheimer’s treatment, this development signals a ray of hope.
What is tau?
Tau, a protein found primarily in neurons, is typically a somewhat innocuous, very soluble protein that stabilizes microtubules in the axon—the part of the neuron that conducts signal to other neurons.
“People think of it as the ties on railroad tracks holding the microtubule tracks together,” Kosik says. However, when soluble, stable tau misfolds—sometimes the result of a mutation of the gene that expresses it—the resulting protein becomes insoluble and tangled, gumming up the works inside the neuron as a neurofibrillary tangle.
In one of several neurodegenerative diseases tau causes, frontotemporal dementia, the frontal and temporal lobes of the brain are impaired, resulting in problems with emotion, behavior, and decision-making.
“Patients do not initially show very many, if any memory problems in this condition,” Kosik says. “They tend to show more psychiatric problems, often with impulsive personalities in which they show inappropriate behaviors.” Other forms in this group of conditions affect language and motor skills.
When researchers took skin cell samples from a few individuals who harbor tau mutations and converted them in vitro into stem cells, and then into neurons, they found that three genes consistently disregulated in those with tau mutations. One of these was of particular interest: RASD2—a gene expressed primarily in the brain that belongs in a family that catalyzes energy-producing molecules (GTPases) and which researchers have studied extensively.
“People had already talked about this gene as possibly involved in Huntington’s disease, which is another neurodegenerative disease,” Kosik says. Researchers consider RASD2 and its more famous cousin RAS (studied heavily in cancer research) “druggable,” Kosik explains.
“There are drugs or potential drugs or small molecules that are out there that could affect the levels of this gene,” he says.
From total failure to possible success
If you’re a neuroscientist interested in tau mutations and cures for the conditions they create, you know a long game lies ahead. The nature of these diseases—genetic and neurological—means that advanced studies must be highly controlled and are often extremely difficult and expensive to come by. In addition, any drugs developed must be both effective and relatively nontoxic.
Such has been the case for Kosik and the paper’s lead author, postdoctoral researcher Israel Hernandez, who have for years studied tau tangles and the protein coding genes that could contribute to or counteract tau misfolding.
Kosik, Hernandez, and their colleagues’ combination of expertise and curiosity led them to examine a GTPase called Rhes, which the gene RASD2 encodes and research has shown to play a role in the development of Huntington’s disease. However, it wasn’t Rhes’s catalytic activity that piqued the researchers’ interest.
“We quickly realized the obvious function of the Rhes protein—its enzyme activity—was not critical to what we were looking for,” Kosik says.
“What we ended up focusing on was the fact that this protein and all members of its family are attached to the cell membrane in a very interesting way,” he continues.
Like its cousins in the Ras superfamily, Rhes is a signaling protein that does its work on the cell surface, where, Kosik explains, a small carbon chain—a farnesyl group—attaches it to the inner membrane through a process called farnesylation.
“There’s an enzyme called farnesyl transferase that takes this protein, Rhes, and attaches it to the membrane, and we decided to focus on that reaction,” Kosik says. “It was a bit of a jump to go in the direction.”
This attachment has been the target of a couple decades and millions of dollars of cancer research under the assumption that if researchers could interrupt the Ras protein connection to the cell membrane, that would interrupt the signals that cause unregulated growth of tumor cells and other cancer behaviors.
“It turns out the drugs in this category, called farnesyltransferase inhibitors, have been tested in humans. They’re safe,” Kosik says. “But, they did not work in cancer.”
Dramatic turnaround
In mice models with frontotemporal dementia, however, it seems they do. And the results are dramatic.
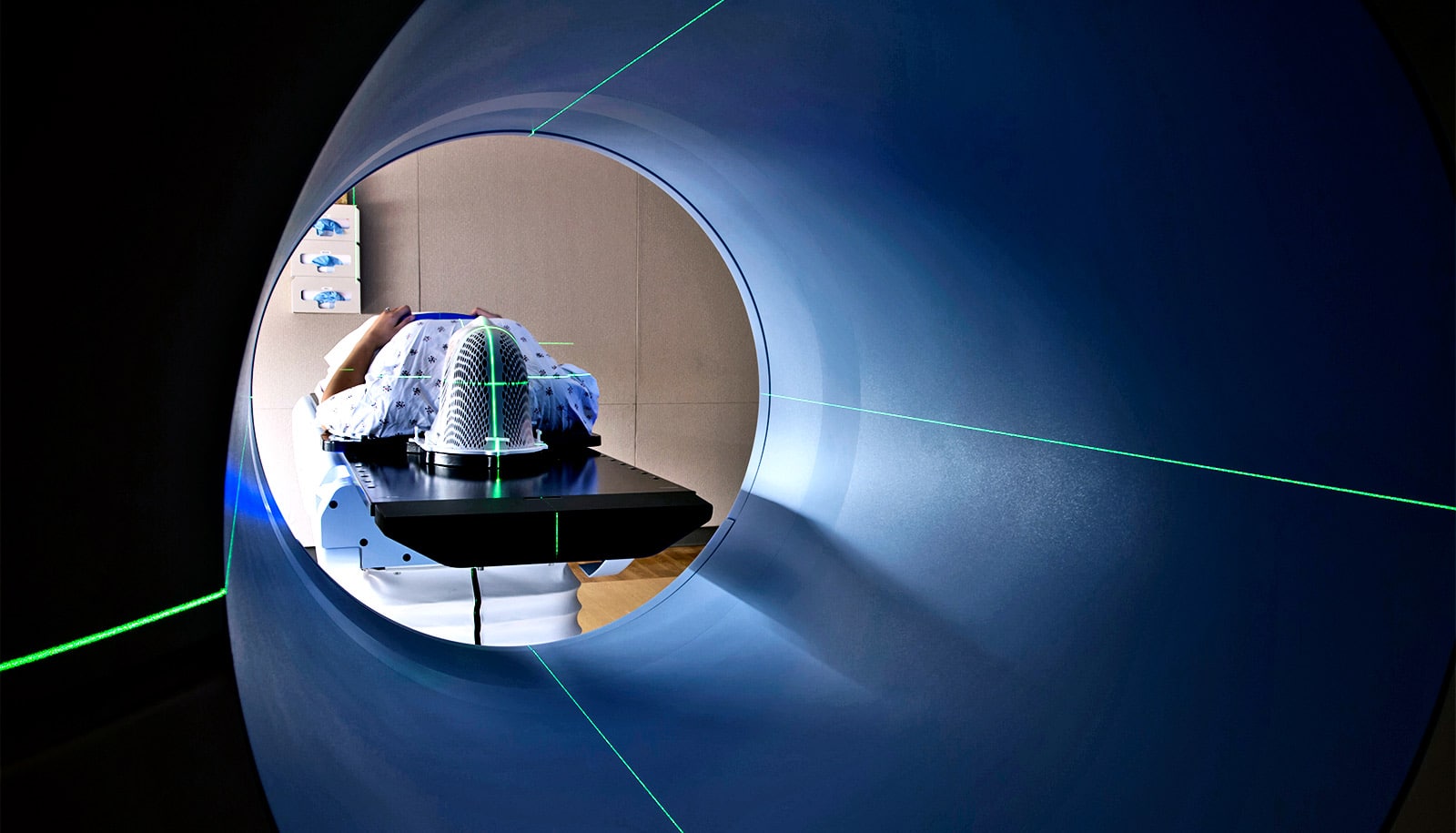
Using the drug Lonafarnib, the researchers treated mice who at 10 weeks were erratic—running around in circles or completely apathetic—and by 20 weeks they were sniffing around their cage or nest building and doing other normal mouse behaviors. Scans revealed the arrest of brain tissue deterioration and inflammation.
Most dramatic: The once-insoluble neurofibrillary tangles reduced greatly, and in some areas including the hippocampus—the memory part of the brain—were nearly completely gone.
“The drug is very interesting,” Kosik says, “It seems to have a selective effect on only the forms of tau that are predisposed to forming the neurofibrillary tangles.”
To prove the drug was targeting the farnsylated Rhes protein, the scientists introduced into the brains of other mouse models an inhibitory RNA gene that specifically suppresses the production of Rhes. And the results completely replicated the effects of the drug.
“This makes us begin to think that although indeed the drug is a general farnesyl transferase inhibitor, one way it’s actually working is by specifically targeting the farnesylation of Rhes,” Kosik says. “And, fortunately, the other farnesyl inhibitions that it’s also doing are not toxic.”
Going forward
The paper represents a milestone in the researchers’ years-long effort to gain ground on the uphill battle that is tauopathic neurodegeneration. As if grueling research wasn’t enough, along the way they have had to search the globe to get the sign-off from a team member who was literally heading uphill—at Mt. Everest.
But the race isn’t over yet. Now the stage is set for human trials, with a few volunteers at risk for the disease. And perhaps further down the road, the team is considering a population with frontotemporal dementia in Colombia where Kosik has conducted similar studies in Alzheimer’s disease.
“We wouldn’t even necessarily do an efficacy study right away,” Kosik says. “We have to just first show that the drug is getting into the human brain and affecting the target.”
But even that early stage may be in limbo. The makers of Lonafarnib, currently in trials for the drug as a treatment for progeria, are reluctant to involve their product in new trials before they get their approvals. Kosik and his team are pondering their options as they contemplate a potential long-awaited solution to a group of heartbreaking—and wallet-draining—neurodegenerative diseases.
“It’s a big challenge,” Kosik says. “I’m working on that.”
Additional researchers from UC Santa Barbara, Harvard Medical School, the Albert Einstein College of Medicine, Washington University, Polish Academy of Sciences, and Icahn School of Medicine at Mount Sinai contributed to the work.
Source: UC Santa Barbara