The common sunscreen ingredient benzophenone-3, also known as oxybenzone or BP-3, can play a role in the development of mammary gland tumors, according to new research in mice.
“Our set of results suggest caution in using BP-3 and the need to dig deeper to understand what it can do in mammary glands and tumorigenesis,” says Richard Schwartz, professor in the microbiology and molecular genetics department at Michigan State University, who has been researching the interaction of diet and cancer cell growth and proliferation for more than 12 years.
“This is the first published result that makes a convincing case that BP-3 can change cancer outcomes.”
The study appears in Oncotarget.
Schwartz and coauthor Sandra Haslam, professor emeritus in the physiology department, previously conducted successful experiments in mouse models that elucidated a relationship between diets high in saturated animal fats with higher incidence and shorter latency of breast cancer.
“We were excited about the results of our diet experiments, but the [the National Institute for Environmental Health Sciences (NIEHS)] was interested in funding a chemical study, so we decided to combine the two,” Schwartz says.
The researchers landed on BP-3, a ubiquitous and easily absorbed chemical. A recent report in the Journal of the American Medical Association found that after just one heavy application of sunscreen, blood levels of BP-3 exceeded the Federal Drug Administration’s guidance for chemicals at a threshold of toxicological concern, and the Centers for Disease Control found BP-3 in 98% of adult urine samples.
BP-3 is also a suspected endocrine disrupting chemical (EDC), substances that interfere with hormonally regulated processes the body uses for a wide range of functions, including mammary gland development.
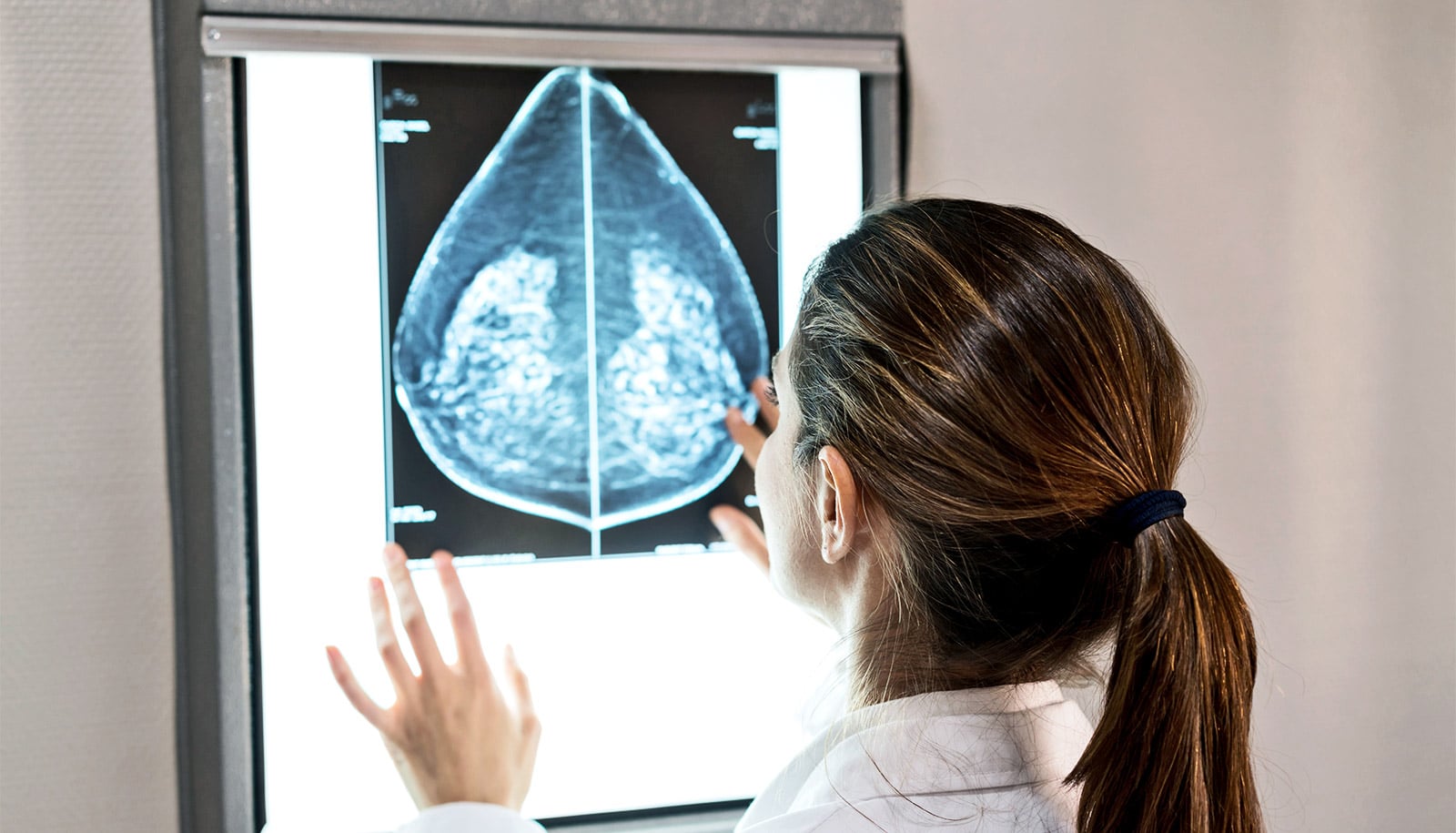
Using a mouse model where the mammary glands lacked a gene often mutated in human breast cancer as a proxy for women growing from puberty into adulthood, the researchers put the mice under three distinct dietary regimes: a lifelong low-fat diet, a high-fat diet during puberty switching to a low-fat diet during reproductive years, and vice versa.
The experiment split mice on these three diets into two groups. One of these groups was fed BP-3 daily at a dose equivalent to a heavy application of sunscreen on a beach day.
Over the course of a year and a half of treatment, the researchers collected tumors from the mice and found robust evidence for the adverse effects of diet and BP-3 on breast cancer development.
“You never know what you’re going to find in experiments like these,” Schwartz says. “I was prepared to see no difference at all from BP-3 in any of our diets, but we found that even a relatively brief exposure to a high-fat diet during puberty is enough to allow BP-3 to cause a change in the outcome for cancer.”
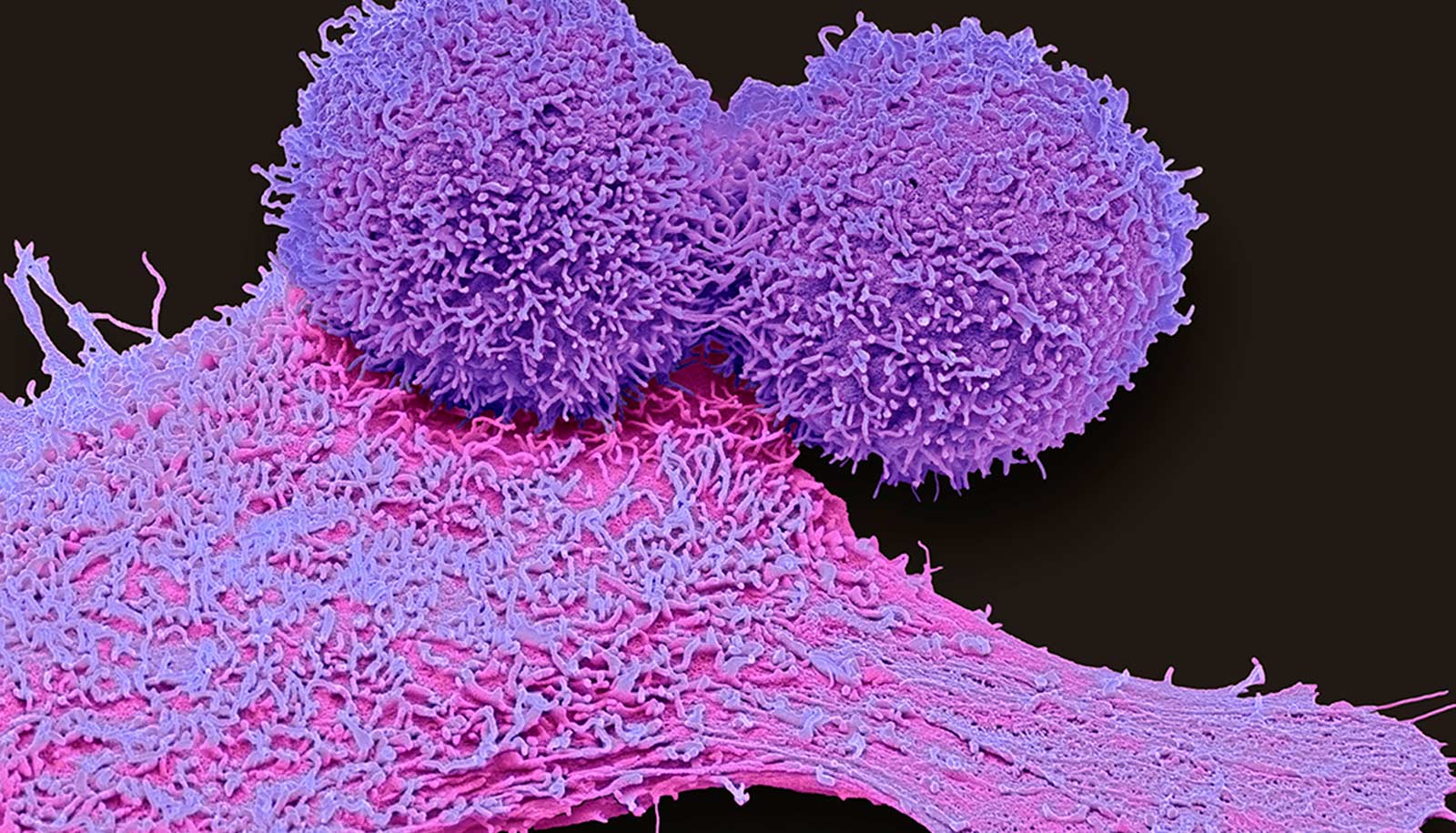
Nearly all mice developed two kinds of aggressive breast cancer tumors. The first, known as epithelial tumors, retain many of the properties of normal mammary gland cells. The second, known as spindle cell tumors, lose most of the properties of normal cells and develop into a deadly, often triple negative form of breast cancer known as claudin-low breast cancer.
The effects of BP-3 varied depending on when the mice were fed a certain type of diet. For example, mice given a lifelong low-fat diet surprisingly acquired some protection against epithelial tumors from the chemical BP-3 but had spindle cell tumors with more aggressive properties. A high-fat diet during puberty, on the other hand, completely blocked any protective effect of BP-3 and caused epithelial tumors to grow more aggressively. The last treatment, a high-fat diet during adulthood, promoted aggressive epithelial tumors.
Interestingly, the researchers also found that before tumors appeared, BP-3 increased the growth of normal breast cells on all diets, a known correlate of more aggressive cancers.
“BP-3 will likely not have the same impact on groups of women with dietary differences, and that’s an important question to ask when designing experiments that study the effects of EDC’s and cancer,” Schwartz explains. “In balance, these results suggest that there are enough bad effects from BP-3 overall that we believe it calls for the precautionary principle.
“When there are alternatives, stay away from BP-3,” recommends Schwartz, who notes that zinc oxide and titanium dioxide creams are good candidates.
The Breast Cancer and the Environment Research Program housed in the National Institute for Environmental Health Sciences (NIEHS) and the National Cancer Institute (NCI) funded the research.
The grant supporting Schwartz’s bench research also encompassed areas of epidemiology and outreach. Epidemiologists at the University of Cincinnati are studying a cohort of young women at varying ages and levels of BP-3 to track any reproduction abnormalities. A breast cancer advocacy group, the Huntington Breast Cancer Action Coalition, is generating messages for women in New York with help from the grant, and Schwartz collaborated with health science communication researchers at Michigan State University.
Source: Michigan State University