A new study uncovers new insights into factors associated with stroke treatment delays and where in the United States patients are more likely to experience slower responses.
When it comes to responding to a stroke, speed is a crucial factor. The longer it takes for someone experiencing a stroke to get to a hospital, the worse the outcome will be. Yet across the United States, delays to treatment can be significant.
The findings, published in the journal Stroke, highlight where interventions should be focused in order to improve stroke outcomes across the country.
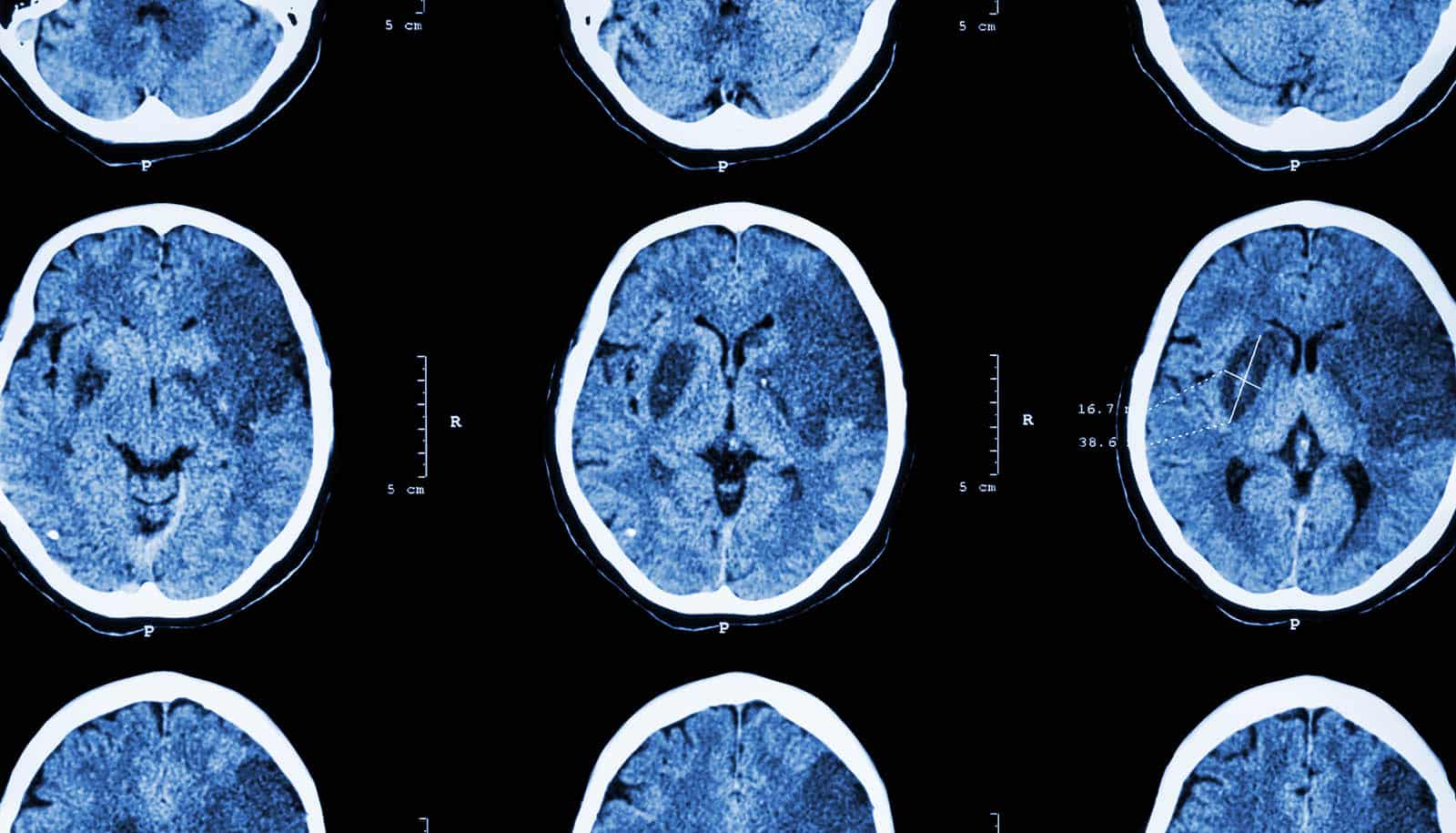
During acute stroke, a blood clot reaches the brain, blocking blood flow and essential oxygen to brain tissue. The longer it takes to restore blood flow, the more tissue will be damaged, leaving patients with reduced abilities in those functions for which the affected brain region is responsible.
Currently, there are two main treatments used in hospitals for patients experiencing a stroke; both aim to break the blood clot and restore blood flow. One involves a medication—a drug called tissue plasminogen activator (tPA)—and the other is a physical approach wherein doctors remove the clot with a tiny tube threaded through a patient’s blood vessels.
“Both are time-dependent,” says Kevin Sheth, professor of neurology and neurosurgery at Yale University School of Medicine and senior author of the new study. “The window to use tPA closes four and a half hours after the stroke. Physical removal is more complicated but can be done up to 12 to 16 hours after the stroke begins. But every minute counts, and even within those windows earlier is better.”
To better understand what factors contribute to treatment delays across the country, the researchers—in collaboration with researchers at Brigham and Women’s Hospital in Cambridge, Massachusetts—used data collected from the “Get with the Guidelines-Stroke” registry, a program launched in 2003 by the American Heart Association that distributes care guidelines and collects data from US hospitals with the aim of improving patient outcomes.
Across nearly 150,000 patients who experienced a stroke between January 2015 and March 2017, 54% arrived at a hospital more than two hours after the onset of stroke symptoms, the researchers found. Compared with patients who arrived earlier, those who took longer were more likely to be older, female, Black, and to have had a mild stroke, findings that align with those of previous studies.
The researchers also looked at community-level social vulnerability. The US Centers for Disease Control and Prevention calculates social vulnerability scores for every US census tract based on socioeconomic factors, household characteristics, and disability, racial and ethnic minority status, and housing type and transportation availability. The scores serve to track factors that adversely affect communities, with higher scores indicating greater vulnerability.
In the study, the researchers found that patients with longer delays to hospital arrival were more likely to live in communities with higher social vulnerability scores. Socioeconomic status, housing type, and transportation availability had the strongest associations with delay.
The researchers also created an interactive map that shows how long it took for patients to arrive at hospitals in different communities nationwide, which they say could be used for targeting interventions.
One important strategy to reduce delays, the researchers say, is the creation of education campaigns.
“The most powerful motivator for going to the emergency department is pain,” Sheth says. “But stroke isn’t usually associated with pain. Plus, neurological symptoms can be weird, leaving people unsure what’s occurring. So informing people about the signs of stroke could help motivate people to seek treatment earlier.”
There have been large-scale education campaigns, Sheth says, but they haven’t made a sizable difference. Campaigns that target communities identified in this study as having longer delays, however, could be more effective.
More ideas for interventions are also needed, says Sheth.
“For how big a problem this is, there hasn’t really been an effort to propose or test new interventions,” he says. “So we need new ideas because the single biggest problem in treating acute stroke is getting people to the hospital fast enough.”
Source: Mallory Locklear for Yale University