Stroke patients are increasingly transferring out of smaller community and rural hospitals and going to larger medical centers for their care and rehabilitation, research finds.
That’s a good thing for patients who need more advanced care—but the trend has drawbacks in terms of cost and highlights a need for more coordination of care between hospitals.
“The underlying goal of stroke care is to get the right person to the right hospital at the right time,” says Benjamin George, a neurologist at the University of Rochester Medical Center and coauthor of a new study in Neurology.
Regional health systems
“The findings of this study show that in recent years community-based hospitals are erring on the side of caution and transferring more patients from their emergency departments to larger hospitals. Given the high cost and burden associated with these transfers, striking a balance between cost and need is essential.”
A national movement toward the formation of large regional health systems has occurred since the passage of the Affordable Care Act and its emphasis on population-based health management. The change has created opportunities and benefits for both small and large hospitals and their patients, such as increased access to specialized care, continuity of care across health systems, and the ability to treat patients closer to home.
In the case of stroke, the creation of regional health networks appears to have accelerated the transfer of these patients away from smaller hospitals.
Researchers used national databases to examine transfer patterns for stroke and transient ischemic attack (TIA) patients from emergency departments of hospitals that serve rural or underserved populations to larger teaching hospitals and academic medical centers. The findings show that national transfer rates had doubled from 2006 to 2014.
Transfers and outcomes
In instances where patients require more advanced care, such as a thrombectomy or neuro-critical care, these inter-hospital transfers are necessary and important. The report also notes that transfer rates vary widely, indicating that some hospitals have developed protocols and strong consultation relationships with specialists in stroke centers that allow them to more effectively evaluate and care for patients in their own emergency rooms.
However, in some instances, such as TIA and certain less severe strokes, transfers don’t automatically produce an improvement in care and result in unnecessary costs and inconvenience to patients and their families.
“…the goal of these partnerships should be, when appropriate, to deliver care that keeps patients closer to home… “
One of the reasons behind the high transfer rates is a general uneasiness on the part of caregivers in smaller hospitals to treat stroke patients. Neurological conditions such as stroke represent the largest category of patients transferred between hospitals—two times greater than trauma, the next largest group.
“Understanding the factors associated with this growth in transfers is necessary in order to build a stroke care system that can economically deliver care, optimize outcomes, and minimize unnecessary costs,” says Adam Kelly, a neurologist at the University of Florida who was a faculty member at URMC when the study took place.
Better coordination
The growth in transfer rates points to the need for better coordination between hospitals to help determine which patients require transfer to stroke centers and those that can be effectively treated where they are.
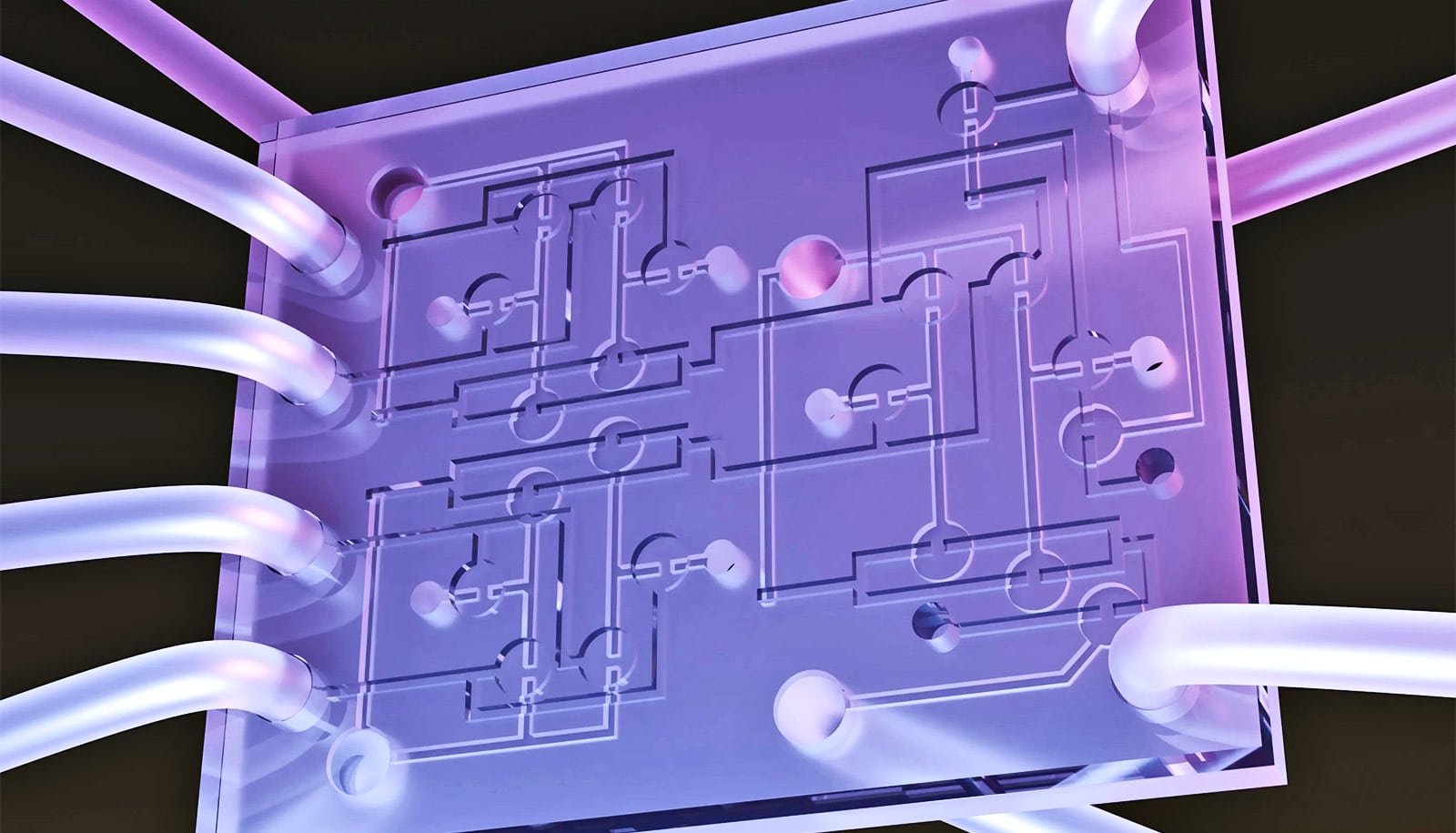
This includes establishing criteria and protocols to evaluate stroke victims and the expanded use of telemedicine—or telestroke—so emergency department providers can consult directly with stroke specialists in other institutions and quickly determine the best course of action.
Can 2nd stroke reopen the recovery window?
“Recent advances in care have transformed the way we treat stroke and the partnerships between hospitals that have formed as a result of the creation of regional health systems has expanded access to that care for more patients,” says coauthor Robert Holloway, chair of the URMC neurology department.
“But the goal of these partnerships should be, when appropriate, to deliver care that keeps patients closer to home and this study shows that on a national level there remains work to be done when it comes to stroke patients.”
Other coauthors are from University of Rochester, Yale University, and Northwestern University.
Source: University of Rochester