Researchers joined forces with NASA to turn stem cells into heart muscle cells.
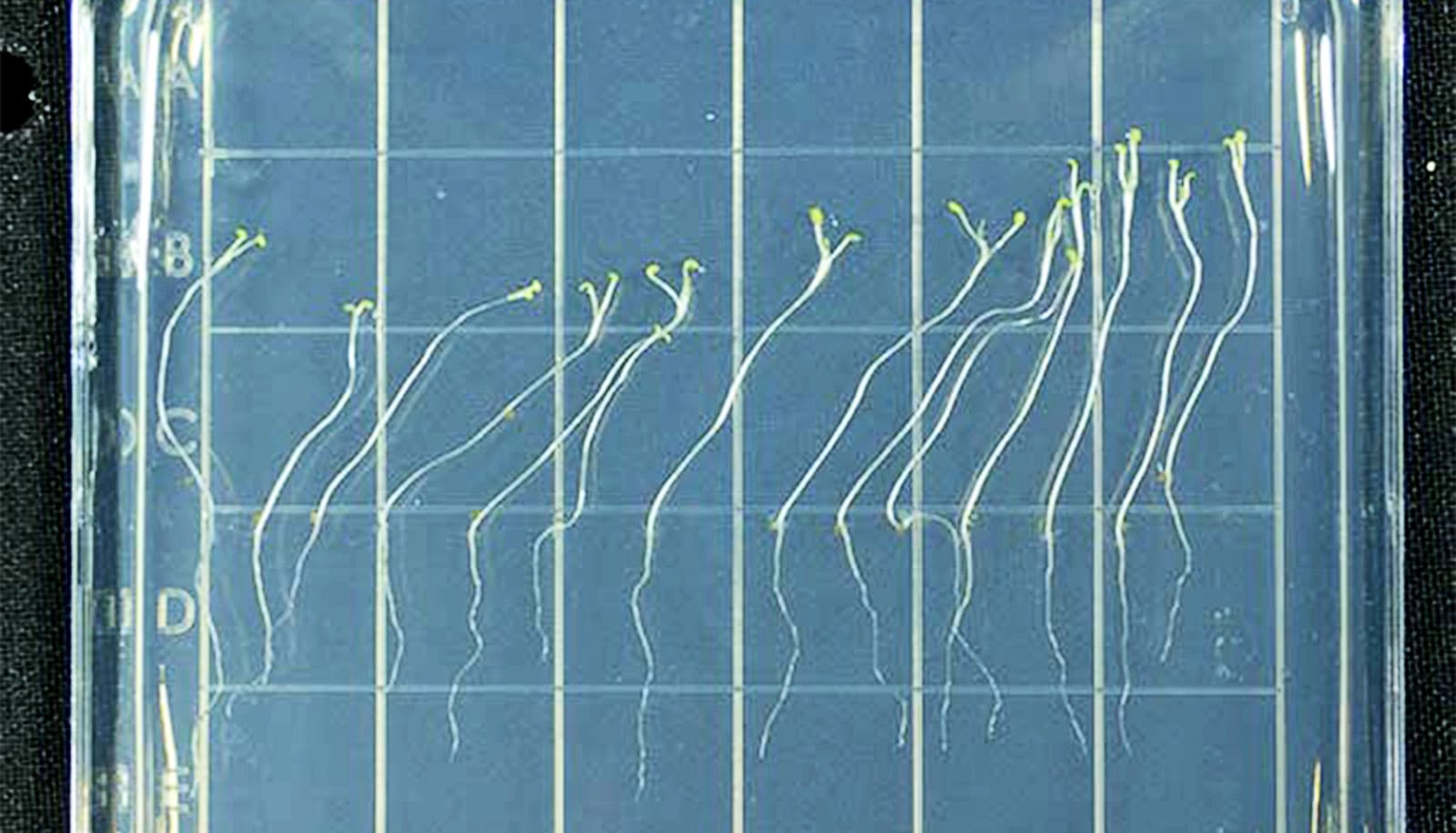
In just three weeks, the stem cells became beating cardiac cells while aboard NASA’s SpaceX-20 mission.
Before trying the real thing on the International Space Station (ISS), the researchers had been using space-simulation machines to enhance the ability of pluripotent, or immature, stem cells to turn into cardiac muscle cells.
The goal was to determine the effects of zero gravity conditions on stem cells and to optimize the generation of clinically relevant cardiac muscle cells on Earth.
Stem cell-derived cardiac muscle cells have been used to treat heart failure in animal models. They’ve also been used to study inherited cardiac diseases separately from the heart of the source patient.
“These cells have the potential to treat heart disease in kids and adults, but repairing a damaged heart requires a large number of heart cells,” says Chunhui Xu, associate professor in the pediatrics department at Emory University School of Medicine. “We were hoping to identify a more effective way to generate these cells by exploring the use of microgravity.”
After the cells that were onboard the space station returned to Earth, the researchers spent the last year diving into the study outcomes.
Their results show that these stem cells grow faster in the zero gravity conditions of space.
“We think about the future of taking care of patients with heart problems,” says Kevin Maher, professor in the pediatrics department and director of the Cardiac Intensive Care Unit at Children’s Healthcare of Atlanta. . “Being able to learn how to make stem cells grow faster has the potential to increase the chance for a better treatment for patients. There’s a lot of work being done to see how we can use these types of stem cells to make the heart stronger in the future.”
The ISS National Laboratory called the spaceflight experiment a significant step for next-generation space research, as freezing cell technology offers many advantages for space research as well as research on Earth.
The potential clinical implications of this research mean that kids and teens with damaged heart valves may instead receive a replacement valve grown from their own cells.
Additionally, cells from a child with heart arrythmia could be taken by biopsy and grown to test medications and treatments, potentially opening a new door to personalized medicine.
The research appears in Biomaterials.
They shared their findings—alongside NASA astronaut Jessica U. Meir—with patients of the Children’s Healthcare of Atlanta Heart Center during a recent event, moderated by Lucky Jain, chair of the pediatrics department of at Emory School of Medicine and chief academic officer for Children’s.
Source: Emory University