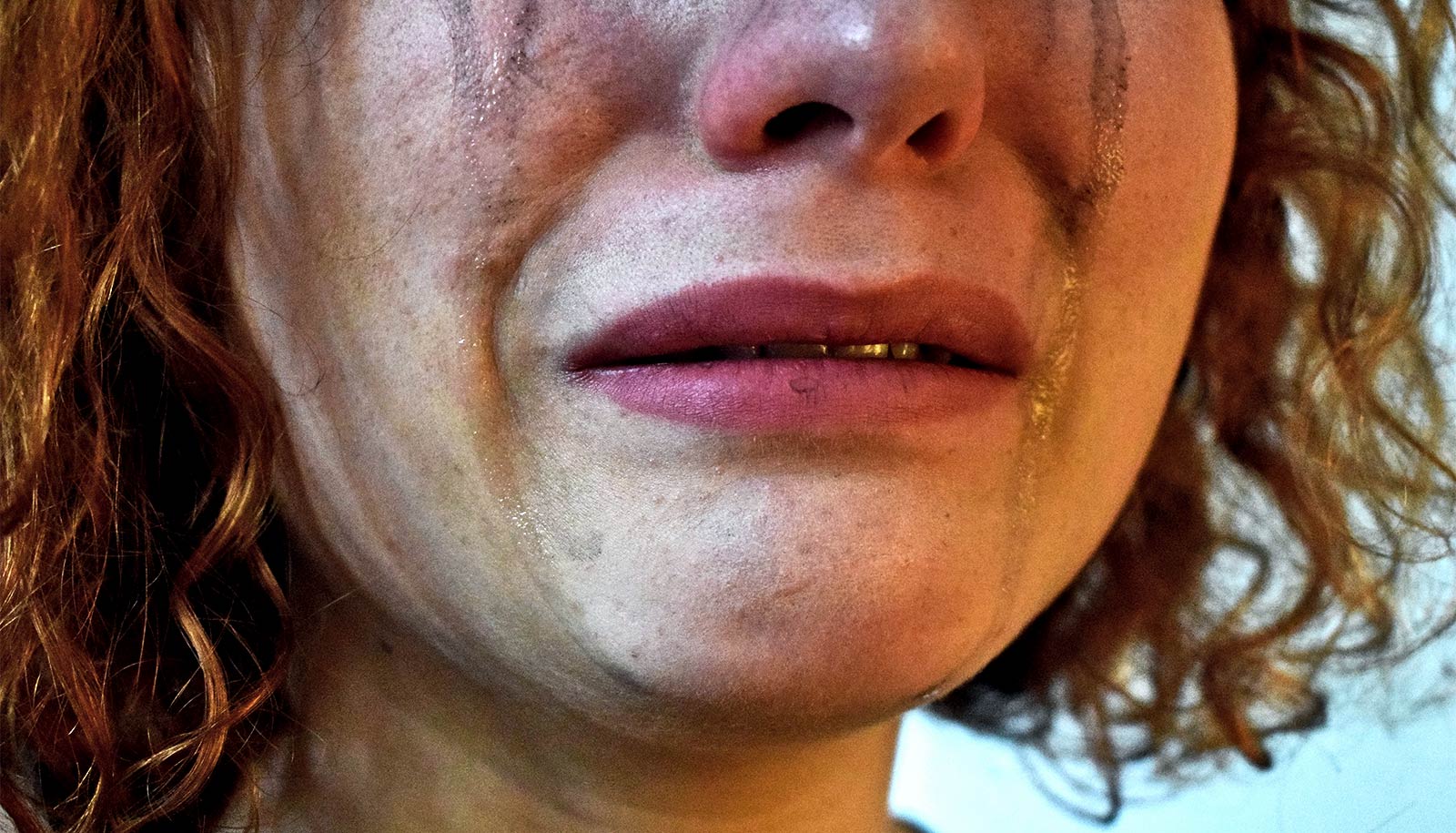
People who have persistent trouble sleeping before the death of a loved one may have an especially difficult time grieving after it, what’s known as “complicated grief,” according to a new study.
Most people who lose a close friend or family member will experience sleep troubles as part of the grieving process, as the body and mind react to the stress of the event, says study coauthor Mary-Frances O’Connor, a professor in the University of Arizona psychology department.
Complicated grief, characterized by a yearning for a lost loved one so intense and persistent that it disrupts a person’s daily functioning, occurs in 7-10% of bereaved people, O’Connor says.
“We know that, for many people, experiencing the death of a loved one is followed by sleep disruption—not surprisingly, given how stressful it is to lose a loved one,” says O’Connor, who directs the university’s Grief, Loss, and Social Stress Laboratory.
“We also know that people who have a more prolonged grief disorder tend to have persistent sleep problems. That led us to ask: What if the reverse is possible? Could it be that people who have had sleep disruption and then experience the death of a loved one are more likely to develop complicated grief?”
Complicated grief symptoms
O’Connor and colleagues looked at data from the multiyear Rotterdam Study, which followed a group of middle-aged and older adults over time and looked at various aspects of their physical and mental health.
The study asked participants to keep sleep diaries documenting the quality of their sleep and to wear a wristwatch monitor, called an actigraph, that objectively measures how long it takes a person to fall asleep, how often a person wakes during the night, and how much time spent in bed is awake versus asleep.
In addition, they also asked participants in interviews if they were still grieving the loss of someone who died in recent months or years. Participants completed follow-up assessments of their grief symptoms.
The researchers compared study participants’ initial responses to what they said approximately six years later, focusing specifically on participants who experienced the loss of a loved one between the first interview and the follow-up.
“What we saw was that if at the first time point you had sleep disruption—both objective and self-reported—you were more likely to be in the complicated grief group than the non-complicated grief group at the second time point,” O’Connor says. “So, poor sleep might not only accompany grief but also be a risk factor for developing complicated grief after a loss.”
History of sleep problems
Sleep is critical for both physical and mental health, which could be why it impacts the grieving process, O’Connor says.
“We know that sleep is important for processing emotional events that happen during the daytime,” she says. “Sleep also helps us to rest and restore our physical body, and grief is a very stressful experience for the body. Being able to rest and restore probably helps us wake up the next day a little more physically prepared to deal with the grief.”
O’Connor says temporary sleep disturbances prior to the death of a loved one—such as stress-induced sleeplessness while caring for a sick family member—are not of as much concern. What is of more concern is a persistent sleep issue, which is more likely to put a person at risk for complicated grief.
O’Connor suggests health care and other support professionals consider sleep history when treating a bereaved person.
“Because grief is such a disruptive and difficult event, doctors often, I think, forget to ask about history when considering how to intervene, rather than just about what’s going on during this intense moment,” she says.
“When physicians and the helping professions are working with bereaved people, they should ask about the history of sleep problems they’ve had, and not just what sleep problems they’re having right now.”
The paper appears in the Journal of Psychiatric Research. Additional coauthors are from Erasmus University Medical Center in the Netherlands and the Phoenix VA Health Care System.
Source: University of Arizona