The mortality rate for pregnant people with sickle cell disease is 26 times higher than the national average, research finds. That figure hasn’t improved since the last time assessment.
Researchers have further documented an association between a substantially higher risk of maternal morbidity and mortality among those with the inherited blood disorder sickle cell disease, compared to those without it.
Their analysis, completed using a large national administrative database with records for pregnant people with sickle cell disease, appears in JAMA Network Open.
A double research disparity
The study findings highlight a need for increased disease-specific interventions for pregnant people with sickle cell disease, or SCD, as well as health disparities long known to affect people with the disorder.
In the United States, the condition is most prevalent in the Black community, according to the US Centers for Disease Control and Prevention. From 2000 to 2003, the maternal mortality rate for people with sickle cell disease was 7.2 deaths per 10,000. In this study looking at data collected 15 years later, the mortality rate among pregnant people with SCD was 13.3 deaths per 10,000.
“People with sickle cell disease are already lacking profoundly needed research and clinical care. Pregnant people with sickle cell disease are at an even greater disadvantage,” says Lydia Pecker, assistant professor of medicine specializing in hematology at the Johns Hopkins University School of Medicine.
Pregnancy with SCD
In the new study, researchers applied the US Centers for Disease Control and Prevention Severe Maternal Morbidity index to the National Inpatient Sample—a nationally representative sample of hospital admissions in the United States. Their analysis covered information collected from 2012 to 2018, which included 5,401,899 deliveries. This figure comprised 3,901 deliveries among pregnant people with SCD and 742,164 deliveries among Black people. 84% of those with sickle cell disease who delivered were Black pregnant people.
Maternal mortality—defined as death during pregnancy, at delivery, or soon after delivery—was highest among those with SCD, at 13.3 per 10,000, compared to 1.2 per 10,000 among pregnant Black people and without SCD and 0.5 per 10,000 among non-Black, non-SCD patients during the study period.
“Pregnancy can bring out negative side effects of any pre-existing condition, and sickle cell disease is no exception,” says Ahizechukwu Eke, associate professor of gynecology and obstetrics at the Johns Hopkins University School of Medicine. “Sickle cell patients require more interventions, including increased blood transfusions, and more frequent ultrasounds to assess the condition of the fetus.”
The researchers note that despite improvements in the care of people with SCD and improvements in the care of high-risk pregnancies, maternal mortality and morbidity rates of people with SCD have not improved. These findings suggest that advancements in SCD and high-risk OB care are not reaching enough pregnant people with SCD, the researchers say.
In the United States, 90% of people with SCD are Black, so pregnancies among people with SCD are often exposed to the harms of systemic and interpersonal racism. These factors contribute to high rates of maternal morbidity and mortality among pregnant Black Americans and, the investigators show, this also affects people with SCD.
“Our work demonstrates that people with sickle cell disease face risk over and above other pregnant people with Black race. Among the risks that are specific to people with sickle cell disease are a highly morbid pre-existing condition and a lack of treatment options, in part due to the insufficient research focused on pregnant people with sickle cell disease and in part to the absence of high-quality specialty care in many regions of the country,” says Macy Early, a fourth-year medical student at Johns Hopkins University School of Medicine, and lead author of this study.
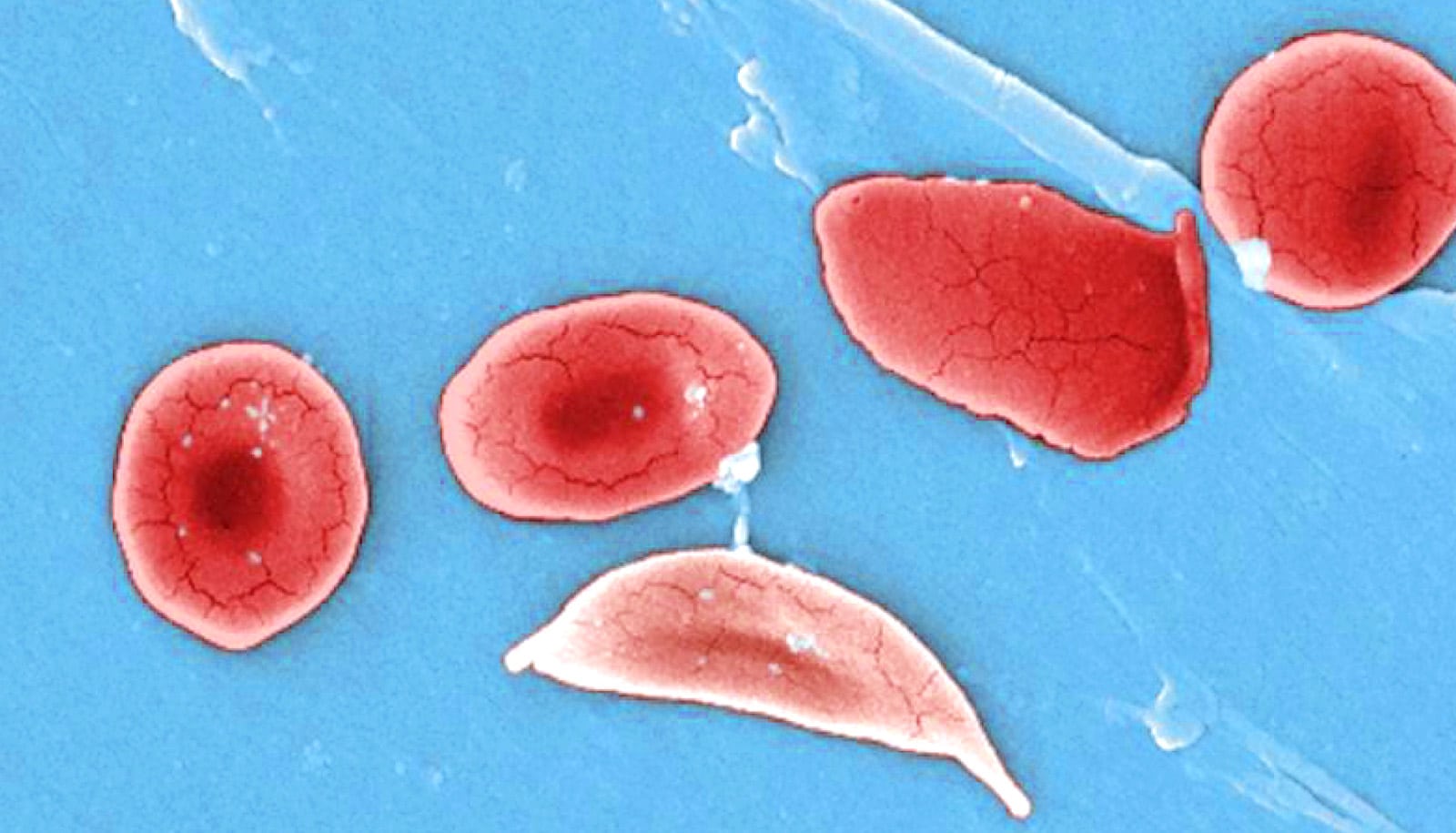
Sickle cell disease
SCD is an inherited blood disorder that is estimated to affect 70,000 to 100,000 Americans. The genetic alteration at the root of the disease affects red blood cells that contain hemoglobin, the protein responsible for transporting and delivering oxygen to the body, to become “sickled” in appearance. The disease not only causes anemia, strokes, organ damage, and shortened life spans, but also repeated and frequent episodes of severe pain when the misshapen red blood cells get stuck in small blood vessels.
Although SCD is a lifelong debilitating illness, advances in treatment have led to nearly all affected people in the United States reaching their reproductive years. As such, there is a growing population of people affected by the effects of SCD in pregnancy and study of possible treatments is needed.
For the pregnant person, SCD is linked to heightened risks of blood clots, chronic pain, anemia, and preeclampsia (high blood pressure during pregnancy). The researchers confirmed that babies born to people with SCD tend to be smaller than average, delivered early, and show damage to the placenta. Data from this study also affirm that SCD is associated with an increased risk of fetal death.
Researchers say they next plan to study data at the individual clinic level to analyze how outcomes for patients differ when high-quality OB care is accessible. They hope to accelerate research on risk and treatment during pregnancy, as well as continue to advocate for funding to ensure that all people in the United States receive high-quality care.
A companion paper to this study comparing outcomes in pregnant people with sickle cell disease and those with nutritional anemia also appears in JAMA Network Open.
Source: Johns Hopkins University