STANFORD (US) — A new collection of compounds—derived from a tiny marine organism—activate hidden reservoirs of HIV that currently make AIDS nearly impossible to eradicate.
Thanks to antiretrovirals, an AIDS diagnosis hasn’t been a death sentence for nearly two decades. But highly active antiretroviral therapy, or HAART, is also not a cure.
Patients must adhere to a demandingly regular drug regimen that carries plenty of side effects. And while the therapy may be difficult to undergo in the United States, it is nearly impossible to scale to the AIDS crisis in the developing world.
[sources]
The problem with HAART is that it doesn’t address HIV’s so-called proviral reservoirs—dormant forms of the virus that lurk within T-cells and other cell types. Even after all of the body’s active HIV has been eliminated, a missed dose of antiretroviral drugs can allow the hibernating virus to emerge and ravage its host all over again.
“It’s really a two-target problem,” says Paul Wender, professor of chemistry at Stanford University, “and no one has successfully targeted the latent virus.”
But, as reported in the journal Nature Chemistry, Wender’s lab is getting closer, exciting HIV patients hoping for a cure.
The lab has created a collection of “bryologs” designed after a naturally occurring, but difficult to obtain, molecule. The new compounds have been shown to activate latent HIV reservoirs with equal or greater potency than the original substance. The lab’s work may give doctors a practical way to flush out the dormant virus.
Nature’s medicine
The first attempts to reactivate latent HIV were inspired by observations of Samoan healers. When ethnobotanists examined the bark of Samoa’s mamala tree, traditionally used by healers to treat hepatitis, they found a compound known as prostratin.
Prostratin binds to and activates protein kinase C, an enzyme that forms part of the signaling pathway that reactivates latent viruses. The discovery sparked interest in the enzyme as a potential therapeutic target, especially as it was discovered that prostratin isn’t the only biomolecule to bind to the kinase.
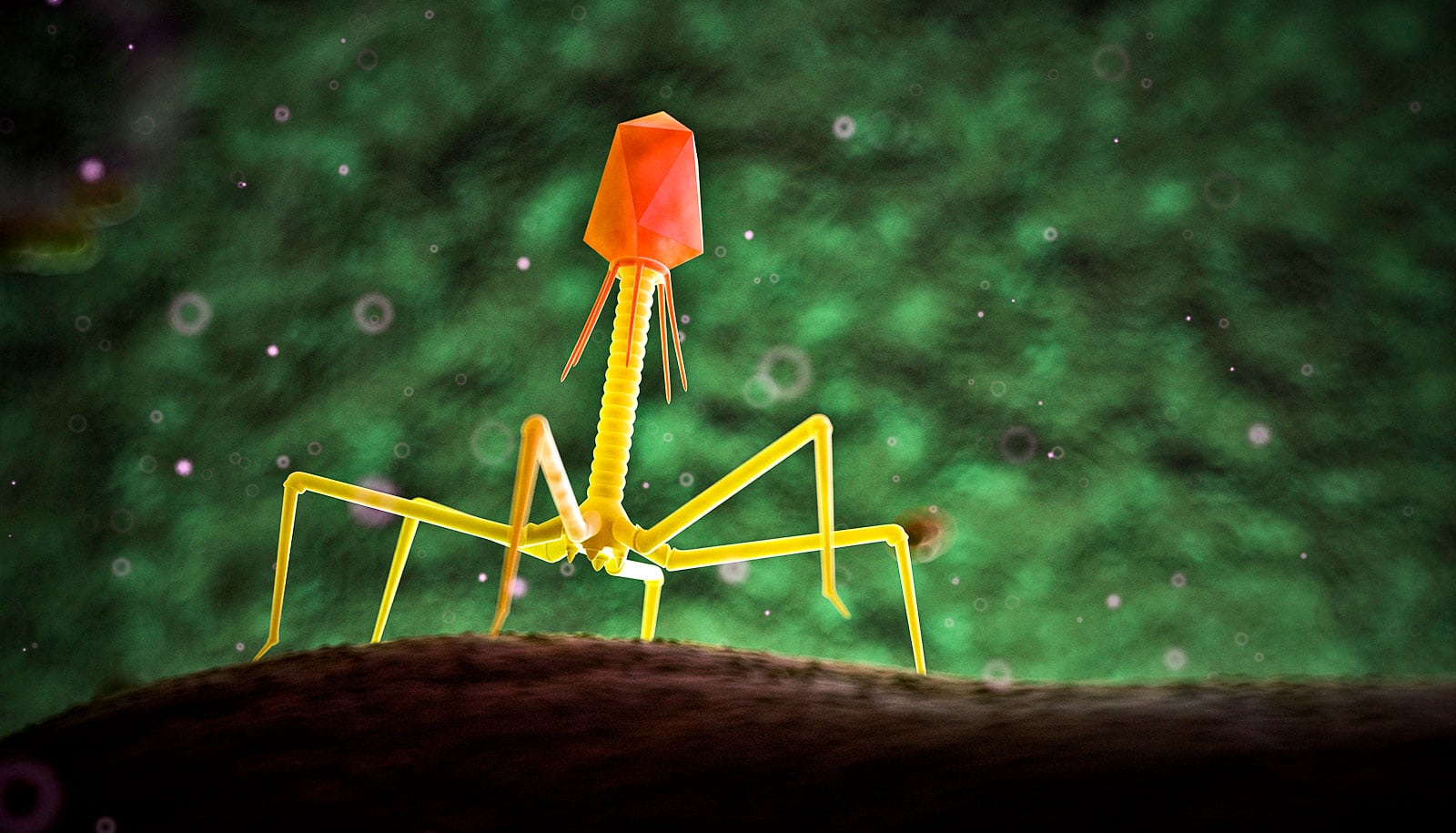
The bryozoan Bugula neritina—a mossy, colonial marine organism—produces a protein kinase C-activating compound that is many times more potent than prostratin. The molecule, named bryostatin 1, was deemed to hold promise as a treatment, not only for HIV but for cancer and Alzheimer’s disease as well.
The National Cancer Institute initiated a Phase II clinical trial for the compound in 2009 for the treatment of non-Hodgkin lymphoma. But the substance had a number of side effects and proved prohibitively difficult to produce.
“It took 14 tons of bryozoans to make 18 grams of bryostatin,” says Wender. “They’ve stopped accrual in trials because, even if the trials worked, the compound cannot be currently supplied.”
Patient enrollment was suspended until more accessible compounds came out of the Wender Group’s lab.
A synthetic approach
Wender, who published the first practical synthesis of prostratin and its analogs in 2008, had set out to make a simpler, more effective synthetic analog of bryostatin.
“We can copy the molecule,” he says, “or we can learn how it works and use that knowledge to create something that has never existed in nature and might be superior to it.”
The seven resulting compounds, called bryologs, share two fundamental features with the original bryostatin: the recognition domain, which directly contacts protein kinase C, and the spacer domain, which allows the bryolog-protein kinase C complex to be inserted into the cell membrane.
The researchers tested the new compounds’ ability to reactivate viral reservoirs in J-Lat cell lines, which contain latent HIV and begin to fluoresce when they express the virus.
In the J-Lat line, bryologs induced virus in as many or more cells than bryostatin at a variety of concentrations, and ranged from 25 to 1,000 times more potent than prostratin. The compounds showed no toxic effects.
Bryolog testing remains in the early stages—the researchers are currently conducting in vivo studies in animal models. But practical bryostatin substitutes may be the first step toward true HIV-eradication therapy.
“I receive letters on a regular basis from people who are aware of our work—who are not, so far as I know, scientifically trained, but do have the disease,” says Wender. “The enthusiasm they express is pretty remarkable. That’s the thing that keeps me up late and gets me up early.”
The research was supported by the National Institutes of Health.
Primary authors are Stanford chemistry graduate student Brian Loy and doctoral students Brian DeChristopher and Adam Schrier, in collaboration with Professor Jerry Zack, co-director of the UCLA AIDS Center, and Matthew Marsden from the UCLA School of Medicine.
More news from Stanford University: http://news.stanford.edu/