An early study shows promise for a new retinal-surgery robot.
When even the most highly trained surgeons perform procedures on the retina—one of the smallest, most delicate parts of the human body—the stakes are high.
Surgeons must account for patients’ breathing, snoring, and eye movements, along with their own involuntary hand tremors, while they work on a layer of cells less than a millimeter thick.
That’s why researchers at the University of Utah’s John A. Moran Eye Center and the John and Marcia Price College of Engineering have collaborated to create a new robotic surgery device that aims to give surgeons “superhuman” hands.
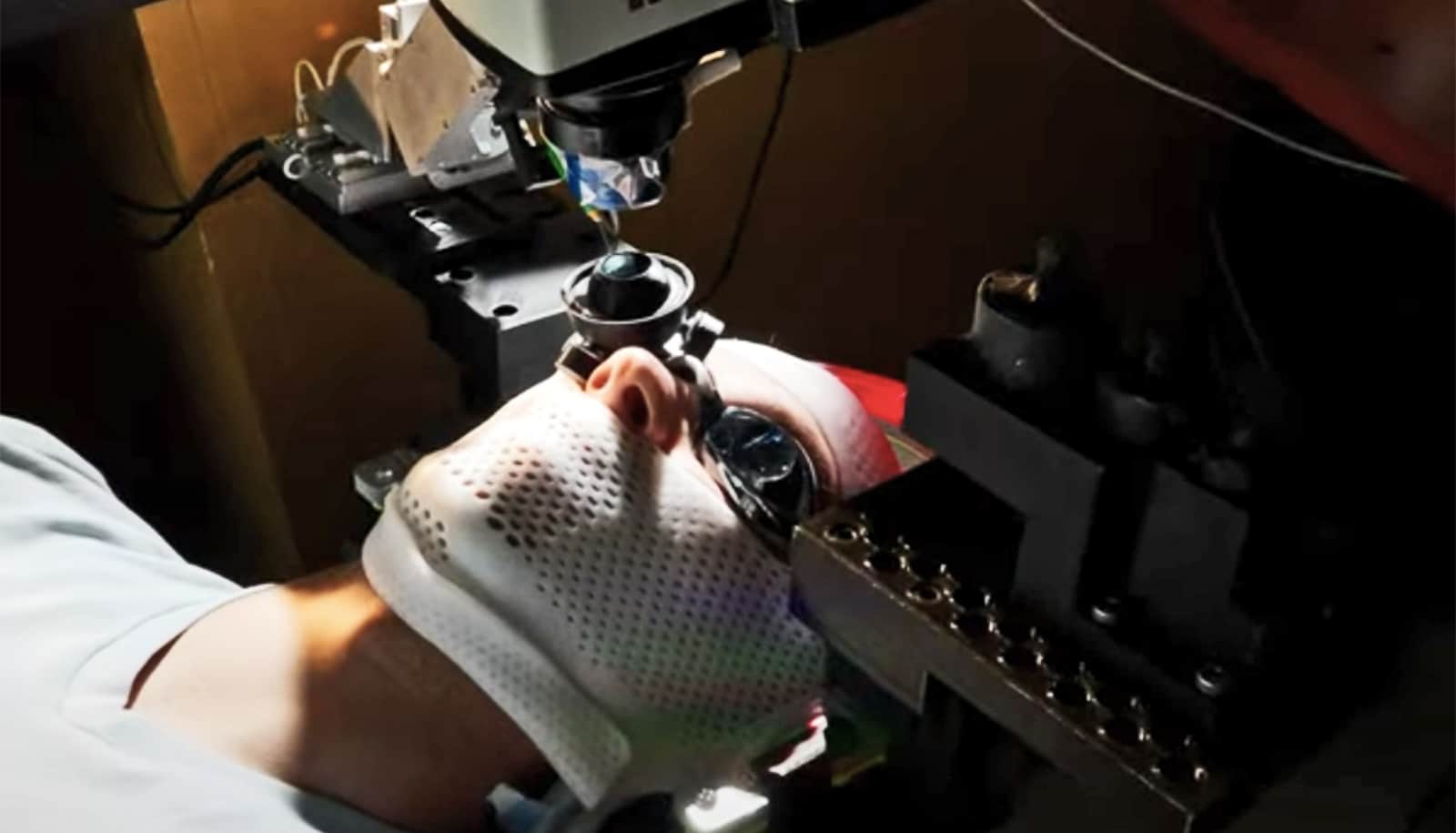
The robot itself is extremely precise, executing movements as small as 1 micrometer (smaller than a single human cell). It is mounted directly to the patient’s head using a helmet, such that subtle (and sometimes not so subtle) movements of the patient’s head are compensated for, keeping the eye quite still from the perspective of the robot.
The robot also scales down the surgeon’s movements, measured using a handheld robotic device known as a haptic interface, to the much smaller surgical site within the eye, compensating for hand tremors along the way.
While still in the testing stages, the device aims to improve outcomes for patients and support cutting-edge procedures, including the delivery of gene therapies for inherited retinal diseases.
The researchers successfully tested the robot using enucleated pig eyes. The study was led by Jake Abbott, a professor in the University of Utah’s mechanical engineering department, and Moran Eye Center retinal specialist Paul S. Bernstein.
The retina is home to the light-sensitive rod and cone cells that form the basis of vision. Several inherited disorders cause those cells to form incorrectly, leading to vision impairments of varying severity, but new gene therapy techniques could reverse those conditions.
“Treatments for vision disorders are rapidly advancing,” Abbott says. “We need to give surgeons better ability to keep up with them.”
The first gene therapy approved by the US Food and Drug Administration for an inherited retinal disease, for example, requires an injection into the space between the retina and another layer of cells known as the retinal pigment epithelium. In addition to the complications presented by eye movement and hand tremors, this subretinal target is vanishingly small; the surgeon must introduce the drug between two submillimeter-thin cell layers.
Because the device is not yet approved to operate on human subjects, testing required a human volunteer fitted with special goggles that allowed an animal eye to be mounted just in front of their natural eye. This allowed the researchers to test the robot’s ability to compensate for head motion and correct for hand tremors, all while operating on animal tissue, at no risk to the volunteer.
In the experiments described in the study, the surgeons achieved higher success rates while using the surgical robot device to perform subretinal injections while also avoiding ophthalmic complications.
These results demonstrate the robot has the potential to improve patient care, according to coauthor Eileen Hwang, a Moran Eye Center retinal surgeon.
“The unique feature of this robot, head mounting, may make it possible for patients to have subretinal injections under intravenous (IV) sedation, rather than general anesthesia,” Hwang says.
“IV sedation allows for faster recovery and is safer in some patients. Robots may also allow for more precise delivery of gene therapy medication compared to manual injections for more reproducible, safer treatments.”
The research appears in the journal Science Robotics.
Additional coauthors are from the University of Southern California’s Keck School of Medicine.
Funding for the research came from the National Eye Institute of the National Institutes of Health, Research to Prevent Blindness, the Las Madrinas Endowment in Experimental Therapeutics for Ophthalmology, and a Knights Templar Eye Foundation Endowment.
Source: University of Utah