High-fidelity computational models of replacement heart valves show that thinner tissues can flap and flutter, which can damage valves and even the blood that flows by, researchers report.
Imagine that you’re in the middle of the aorta, the body’s pipeline for oxygen-rich blood, looking back toward the heart’s primary pump, the left ventricle.
The ventricle muscle contracts and the aortic heart valve’s three leaflets explode open and blood flows by at up to 200 centimeters (78.74 inches) a second.
Those three leaflets are flapping in the flow—fluttering, in engineering terms. That’s a problem. It could lead to leaflet tearing, calcium deposits, fatigue failure, and even damage the flowing blood.
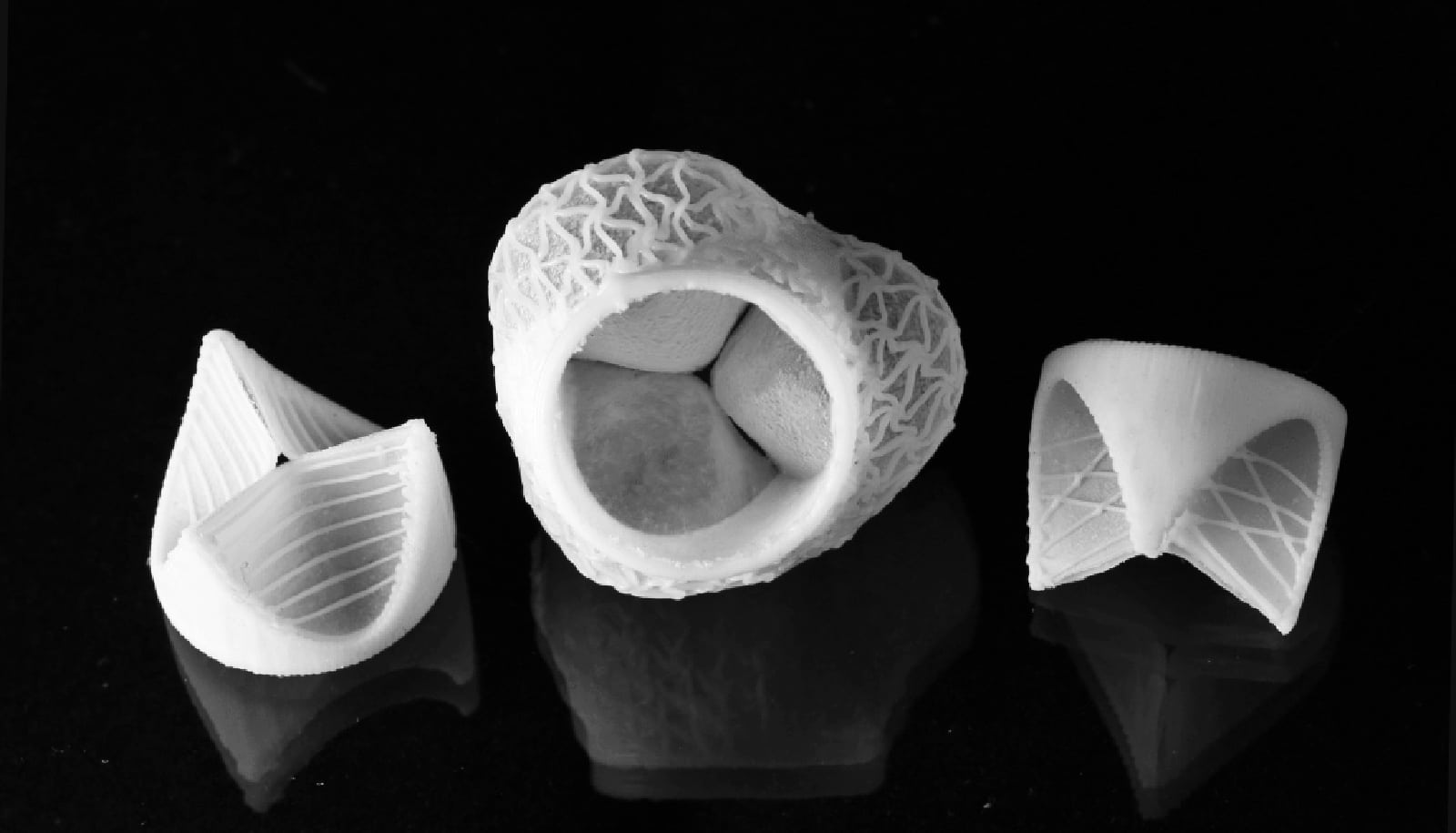
The video shows computer models of replacement aortic heart valves. The models show biological tissues built into the valves at thicknesses of 100%, 75%, 50%, and 25%. You can see fluttering in the thinner tissues at the bottom. (Credit: Ming-Chen Hsu)
Now we have an eyewitness look, from a physically impossible point of view, thanks to computational models of the fluid-structure interactions of blood and heart valves the researchers created. A paper covering the work appears in the Proceedings of the National Academy of Sciences.
Thin isn’t necessarily better
The researchers used their technology to study what happens when patients receive thinner and thinner biological tissues from cows or pigs in transcatheter aortic valve replacement.
The procedure involves collapsing an artificial valve into a catheter that is threaded through an artery to the aortic root, where it expands and secures itself in place.
It makes sense to choose thin tissues when building the replacement valves—thinner tissues can fold into smaller catheters for easier movement through the narrow tubes of the arteries.
But, in side-by-side models comparing tissue thicknesses of 100%, 75%, 50%, and 25%, researchers saw problems with the two thinner options.
It’s not easy to develop a predictive computational model of a heart valve in action, says Ming-Chen Hsu, an associate professor of mechanical engineering at Iowa State University, who has modeled heart valves for more than five years.
There’s constant contraction, pressure, and flow. The valves are flexible. It’s a highly dynamic system, with a lot of variables.
“We’re really modeling the whole physiological system,” Hsu says. “That’s why it has taken several years to correctly model the blood flows, which can change from laminar to turbulent, the heart valves, which are very thin and nonlinear, and the multi-physics coupling, which can be numerically unstable.”
Look at the science
This kind of modeling takes supercomputing power, Hsu says. He and colleagues simulated the valves in the study using computing resources at the Texas Advanced Computing Center, with each cardiac cycle taking about two days to run on 144 processing cores.
But this is a problem worth the time and effort. Any time a replacement heart valve wears out, patients face another heart procedure. That makes avoiding leaflet flutter in a replacement valve a “crucial quality criterion,” the engineers write in the study.
Hsu credits Emily L. Johnson, a doctoral student his lab who also works on wind turbine modeling, with helping him take his lab’s work further in a new direction.
“My background is in computational methods,” he says. “But students suggested we should look more at the science questions, too. We’re not just developing computational tools anymore.”
80x more flutter energy
In this case, the computer models and resulting videos make the science easy to see and understand. “I think videos are the best way to show our results,” Hsu says.
When thrown open by a pumping heart, the thinner leaflets buckle in the middle and flutter in the blood flow. “It’s like a flag flapping,” Johnson says.
The engineers were able to quantify the flapping and found that thinner tissues had as high as 80 times more “flutter energy” than thicker tissues.
The resulting conclusions are clear as the engineers’ views of the fluid-structure interactions inside a heart valve: “Considering the risks associated with such observed flutter phenomena, including blood damage and accelerated leaflet deterioration, this study demonstrates the potentially serious impact of introducing thinner, more flexible tissues into the cardiac system.”
Additional coauthors are from the University of Texas at Austin and Iowa State University. The National Institutes of Health supported the work.
Source: Iowa State University