A new technique uses light to activate a drug stored in circulating red blood cells so that it is released exactly when and where it is needed.
The work, which overcomes a decades-long scientific hurdle in drug delivery, could drastically reduce the amount of a drug needed to treat disease—and therefore its side effects, too.
“Using light to treat a disease site has a lot of benefits beyond the isn’t-that-cool factor.”
“Using light to treat a disease site has a lot of benefits beyond the isn’t-that-cool factor,” says study leader David Lawrence, professor in the University of North Carolina at Chapel Hill’s Eshelman School of Pharmacy. “Those benefits could include avoiding surgery and the risk of infection, making anesthesia unnecessary, and allowing people to treat themselves by shining a light on a problem area, such as an arthritic knee.”
The research appears in the journal Angewandte Chemie.
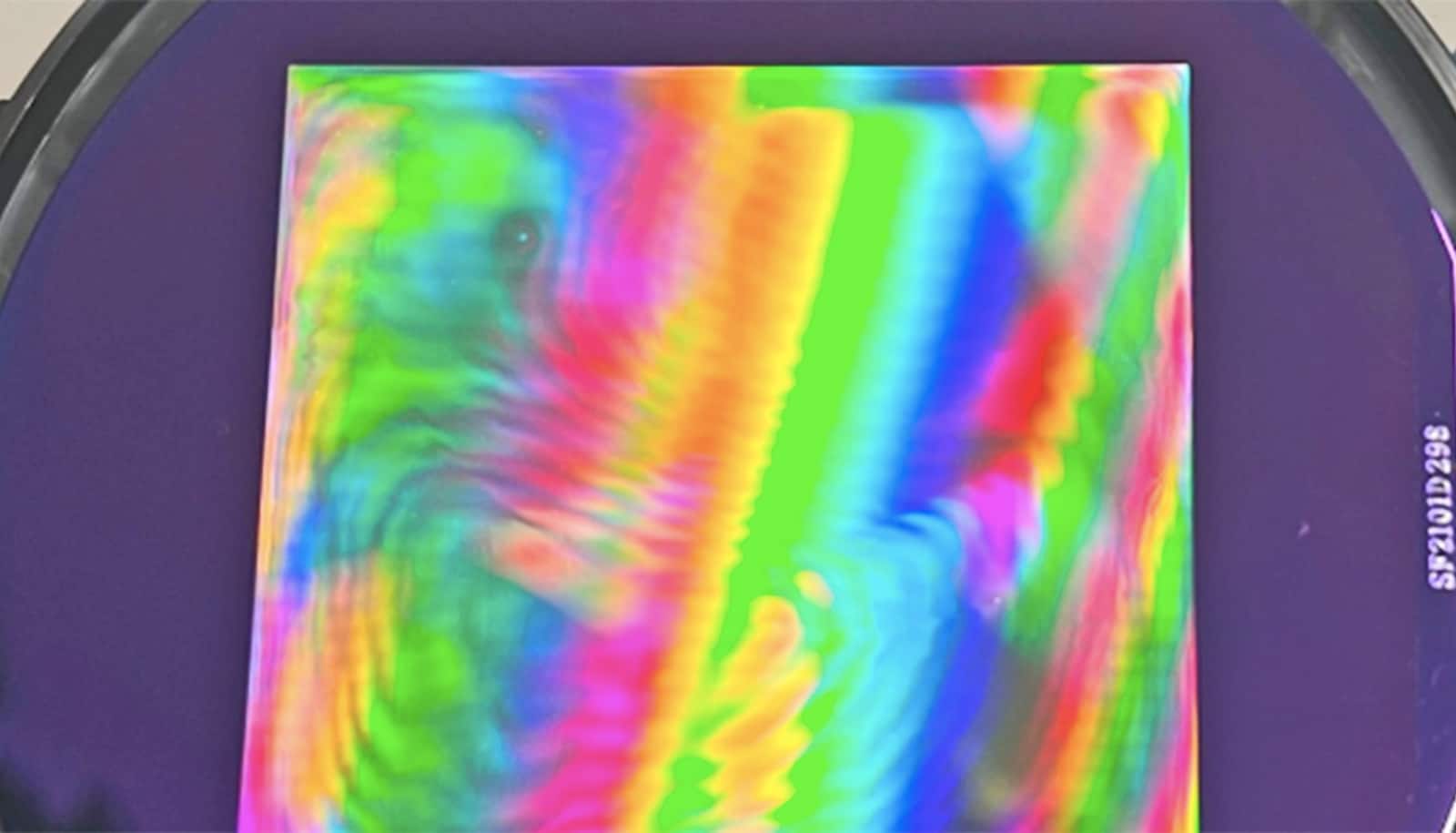
Lawrence and his team attached a drug molecule to vitamin B12 and loaded the compound into red blood cells, which can circulate for up to four months, providing a long-lasting reservoir of medicine that can be tapped as needed. They then demonstrated their ability to overcome a longtime technical hurdle: using long-wavelength light to penetrate deep enough into the body to break molecular bonds—in this case, the drug linked to vitamin B12.
Ultrasound and bubbles prick cells for gene therapy
But there was another hurdle: Long-wavelength light can penetrate much more deeply into the body, but it doesn’t carry as much energy as short wavelength light, and cannot typically break molecular bonds. To activate the drug with long-wavelength light, Lawrence and his team had to figure out how to do it in a way that required less energy.
“That’s the trick, and that’s where we’ve been successful,” says Lawrence.
Lawrence’s team solved the energy problem by introducing a weak energy bond between vitamin B12 and the drug and then attached a fluorescent molecule to the bond. The fluorescent molecule acts as an antenna, capturing long wavelength light and using it to cut the bond between the drug and the vitamin carrier.
Pill could deliver insulin without the pain
Lawrence points to some complex and deadly cancers where physicians might have a better chance of helping the patient if a wide array of anti-cancer agents could be used.
“The problem is when you start using four or five very toxic drugs you’re going to have intolerable side effects,” he says. “However, by focusing powerful drugs at a specific site, it may be possible to significantly reduce or eliminate the side effects that commonly accompany cancer chemotherapy.”
Lawrence has also created a company in partnership with UNC, Iris BioMed, to further develop the technology to be used in humans. Lawrence is a member of the UNC Lineberger Comprehensive Cancer Center and professor in the College of Arts and Sciences and School of Medicine.
Source: UNC Chapel Hill