A new interface that connects a leg prosthesis with the residual nerves in the user’s thigh allows above-the-knee amputees to feel their prosthetic foot and knee in real time, a new study shows.
While walking, people with intact legs feel when they move their knee or when their feet touch the ground. The nervous system constantly draws on sensory feedback of this sort to precisely control muscles. People using a leg prosthesis, however, don’t know precisely where the prosthesis is located, how it is moving, or what type of terrain it is standing on.
They often cannot trust their prosthesis completely when walking, leading them to rely too often on their intact leg, which in turn reduces their mobility and causes them to tire quickly. A simple walk on pebbles or sand, for example, can prove very exhausting for people using a prosthesis.
Furthermore, people with amputations can experience phantom limb pain, a condition that existing medications often cannot treat.
Savo Panic, a volunteer fitted with the device, says he wakes up at night due to the phantom pain: “The toe that I don’t have hurts. My big toe, foot, heel, ankle, calf—they all hurt, and I don’t even have them.”
The new prosthesis benefited the amputees in a variety of ways, the researchers report in Nature Medicine.
“This proof-of-concept study shows how beneficial it is to the health of leg amputees to have a prosthesis that works with neural implants to restore sensory feedback,” says Stanisa Raspopovic, a professor at the Institute of Robotics and Intelligent Systems at ETH Zurich.
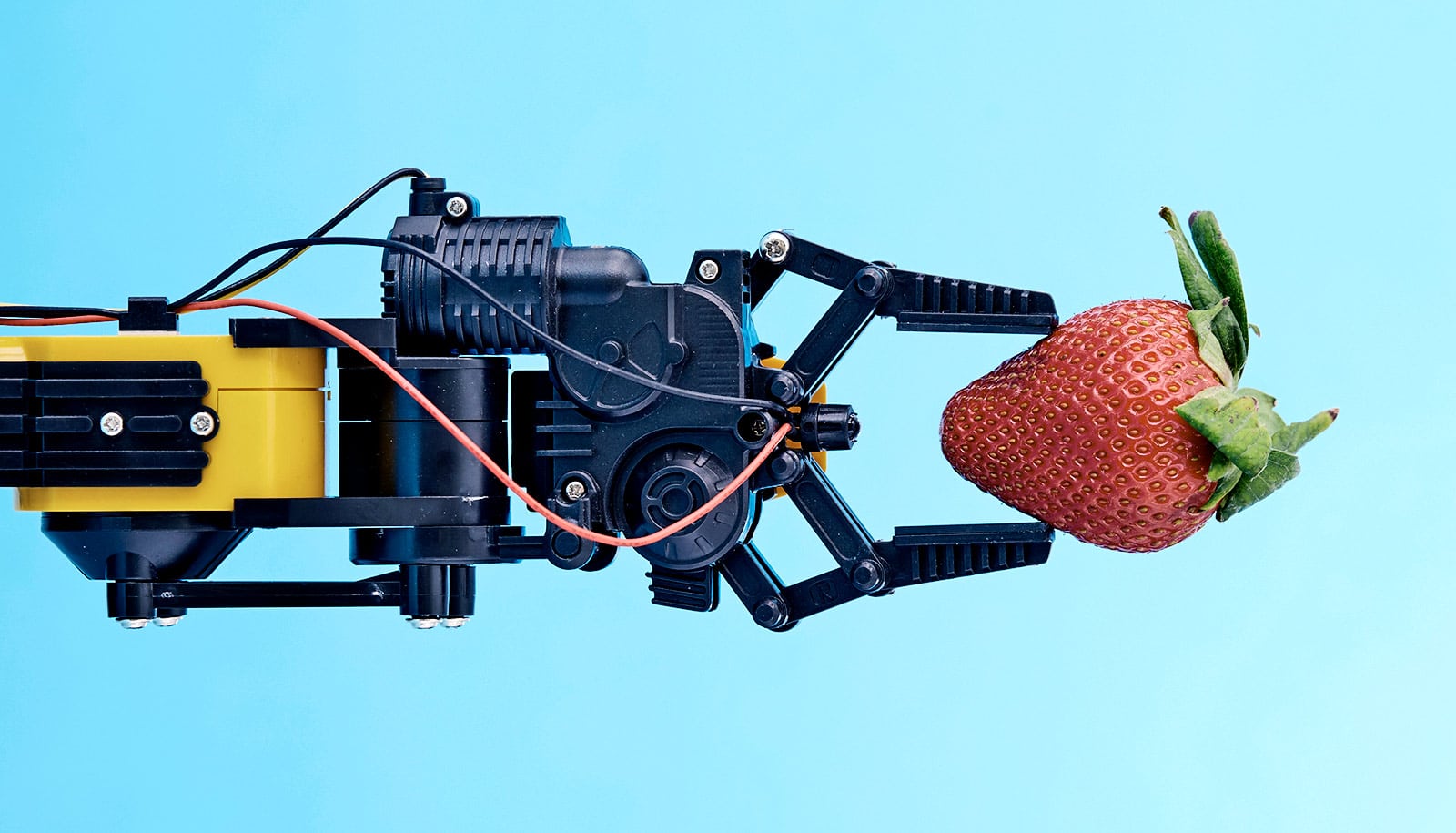
Tactile and motion sensors
To provide the nervous system with sensory information, the scientists began with a commercially available high-tech prosthesis: they attached tactile sensors to the sole of the prosthetic foot, and collected the data on knee movement provided by the prosthesis’s electronic knee joint.
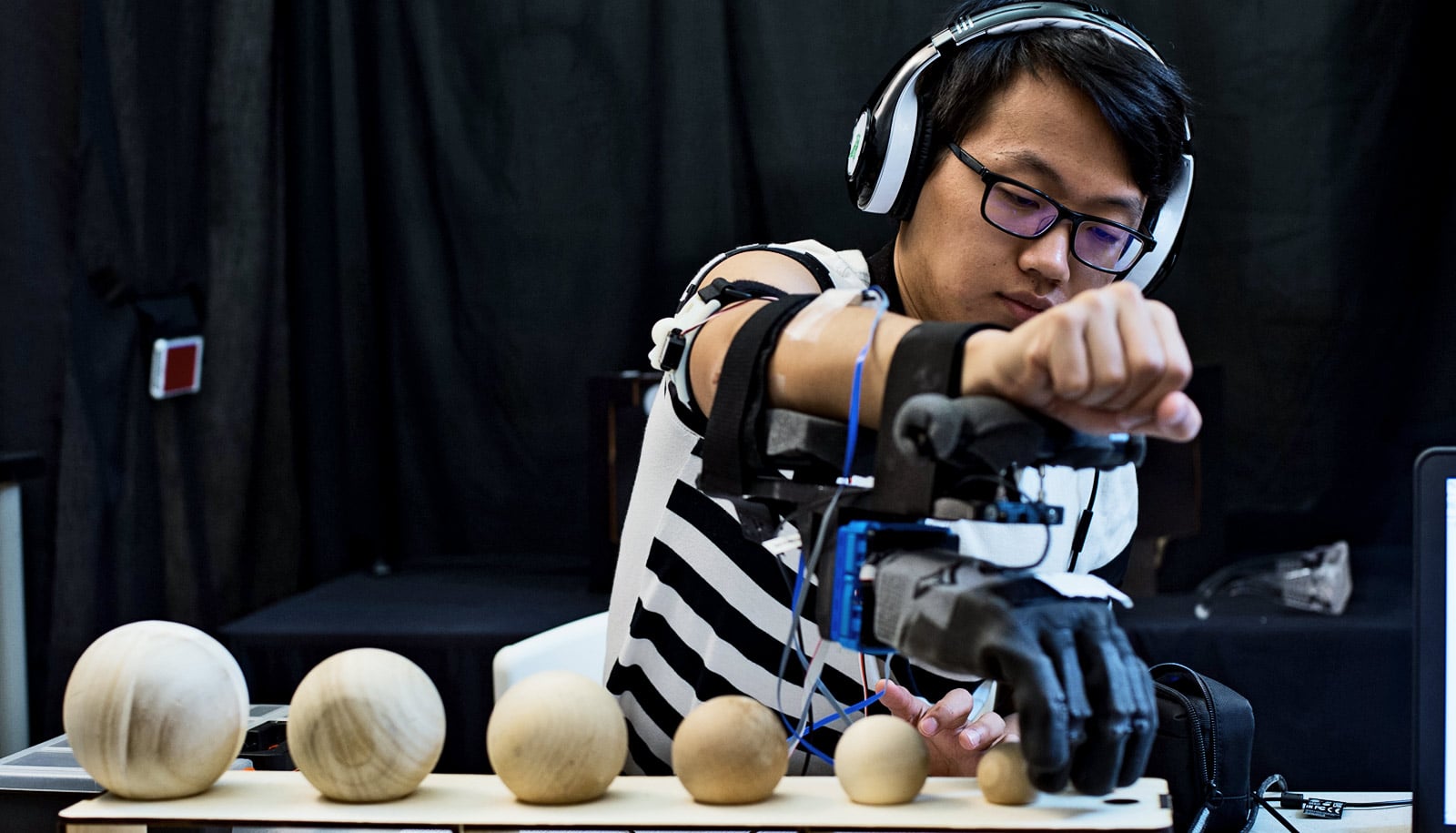
For the three months that the experiment lasted, surgeons placed tiny electrodes in each volunteer’s thigh and connected them to the residual leg nerves.
“The goal of the surgery was to introduce electrodes in the right places inside the nerve to allow the restoration of lifelike sensory feedback, and to allow the stability of the electrodes,” says Marko Bumbasirevic, professor and orthopedic microsurgeon at the Clinical Centre of Serbia in Belgrade, who was the clinician responsible for the electrode implant. Scientists at the University of Freiburg developed the electrodes and the prosthesis came from the prosthetic company Össur; both actively involved in the project.
The research team developed algorithms to translate the information from the tactile and motion sensors into impulses of current—the language of the nervous system—which went to the residual nerve. Then nature does the rest: the signals from the residual nerves are conveyed to the person’s brain, which can sense the prosthesis and helps the user adjust their gait accordingly. The machine and the body are finally connected.
Walking on sand
As part of the study, the volunteers underwent a series of tests—alternating trials with and without neurofeedback. The results made it very clear just how advantageous the feedback was: walking with neurofeedback was physically much less demanding, evident from the significant reduction in the volunteers’ oxygen consumption while walking.
Also, brain activity measurements during the trials showed walking with neurofeedback was also less strenuous mentally for the volunteers, who didn’t have to concentrate as hard on their gait, which meant that they were able to devote more of their attention to other tasks.
In one difficult test, the volunteers had to walk over sand—and the feedback enabled them to walk considerably faster. In surveys, the volunteers said the neurofeedback greatly increased their confidence in the prosthesis.
‘I don’t feel any phantom pain’
The interface with the nervous system can also stimulate the nerves independently of the prosthesis. Before they started the trial, both volunteers complained of phantom limb pain. Over the course of a one-month therapy program with neurostimulation, the scientists managed to considerably reduce this pain in one of the volunteers.
Panic said his pain disappeared completely. “Since I have started this treatment program, after having received electrical stimulations, I don’t feel any phantom pain.”
While the scientists view these outcomes optimistically, they point out the need for a longer investigation with in-home assessments and a greater number of volunteers, in order to provide more robust data that they can use to draw more significant conclusions.
For the time-limited clinical study, the signals from the prosthesis moved along cables through the skin to the electrodes in the thigh. This meant that the volunteers had to undergo regular medical examinations. To eliminate this need, the scientists intend to develop a fully implantable system.
“At SensArs, we’re planning to develop a wireless neurostimulation device that can be fully implanted into the patient like a pacemaker, and that can be brought to the market,” says Francesco Petrini, CEO of SensArs.
Additional researchers from EPFL, the Sant’Anna School of Advanced Studies in Pisa, the University of Montpellier, and the company mBrainTrain contributed to the project.
Source: ETH Zurich