Adding a pre-ketone supplement, a component of a high-fat, low-carb ketogenic diet, to a type of cancer therapy in a laboratory setting was highly effective for treating prostate cancer, researchers report.
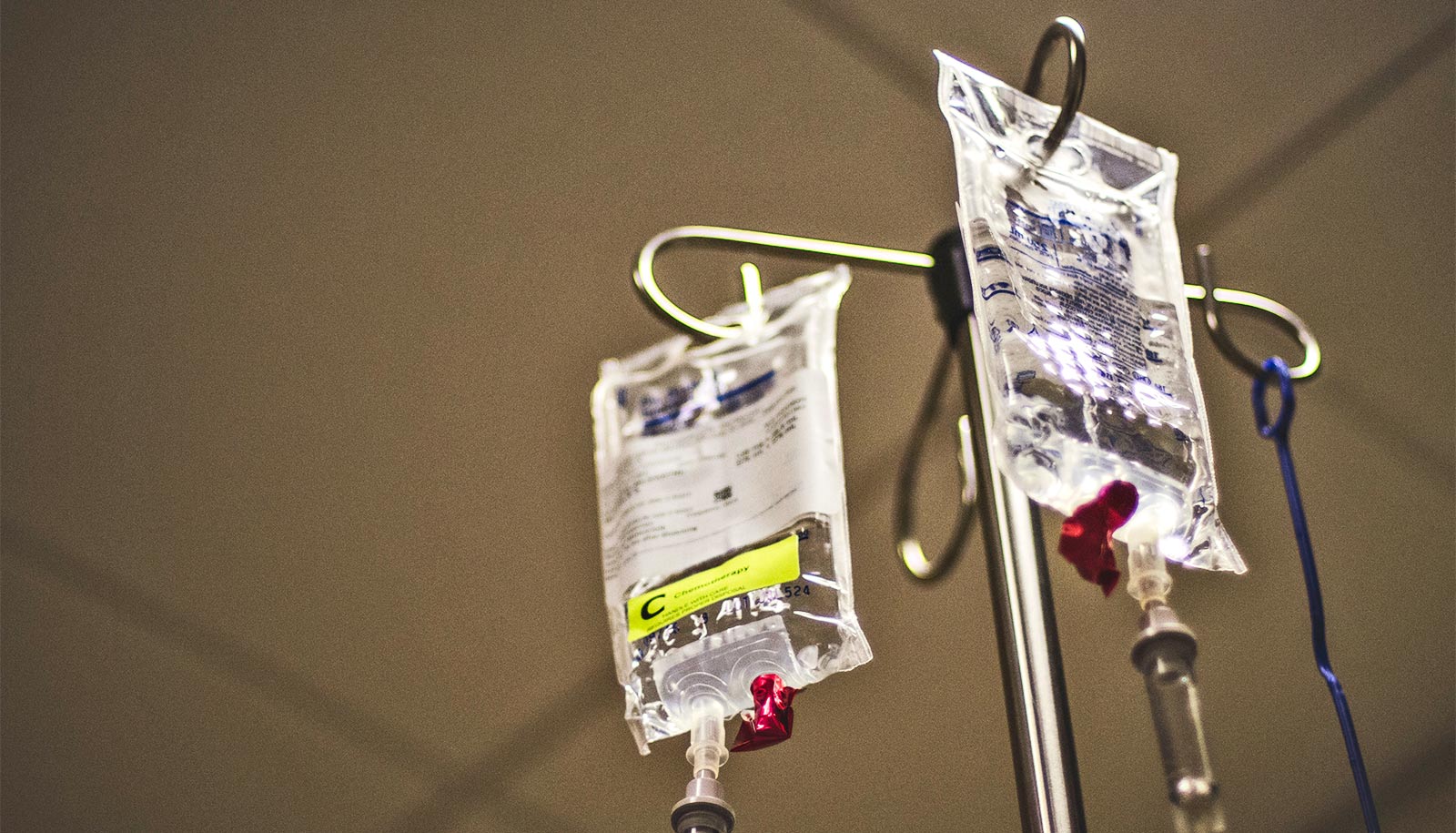
As reported in the journal Cancer Research, the researchers tackled a problem oncologists have battled: Prostate cancer is resistant to a type of immunotherapy called immune checkpoint blockade (ICB) therapy. ICB therapy blocks certain proteins from binding with other proteins and paves the way for our body’s fighter cells, T cells, to kill the cancer.
“Prostate cancer is the most common cancer for American men, and immunotherapy has been really influential in some other cancers, like melanoma or lung cancer, but it hasn’t been working almost at all for prostate cancer,” says Xin Lu, associate professor in the biological sciences department at the University of Notre Dame, who is affiliated with the Boler-Parseghian Center for Rare and Neglected Diseases.
Adding a dietary supplement might overcome this resistance, suggests lead author Sean Murphy, a 2024 alumnus who was a doctoral student in Lu’s lab and had been following a keto diet himself.
Knowing that cancer cells feed off of sugar, he decided that depriving mouse models of carbohydrates—a key component of the keto diet—might prevent cancer growth.
He divided the models into different groups: immunotherapy alone, ketogenic diet alone, a pre-ketone supplement alone, the ketogenic diet with the immunotherapy, the supplement with the immunotherapy, and the control.
While the immunotherapy alone had almost no effect on the tumors (just like what happens to most patients with prostate cancer), both the ketogenic diet with the immunotherapy and the pre-ketone supplement with the immunotherapy reduced the cancer and extended the lives of the mouse models.
The supplement with the immunotherapy worked best.
“It turned out this combination worked really well,” Lu says. “It made the tumor become very sensitive to the immunotherapy, with 23% of the mice cured—they were tumor-free; in the rest, the tumors were shrinking really dramatically.”
The evidence points to the possibility that a supplement providing ketones, which are what is produced in the body when people eat a keto diet, might prevent the prostate cancer cells from being resistant to immunotherapy. This may lead to future clinical studies that examine how ketogenic diets or keto supplements could enhance cancer therapy.
While keto diets allow for minimal carbohydrates, the success of this study is not about the lack of carbohydrates, Murphy and Lu stress. It is about the presence of the ketone body, a substance produced by the liver and used as an energy source when glucose is not available. The ketones disrupt the cycle of the cancer cells, allowing the T cells to do their job to destroy them.
The discovery was also exciting on a molecular level, Lu says. Any type of dietary study can suffer from the potential issue of causation: Are the results from the diet or other changes made because of the diet? But Lu and his collaborators confirmed their results using single-cell RNA sequencing, which examines the gene expression of single cells within the tumor.
“We found that this combination of the supplement and the immunotherapy reprogrammed the whole immune profile of the tumors and recruited many T cells into the tumors to kill prostate cancer cells,” Lu says.
The successful therapy also reduced the number of a type of immune cell called neutrophils. Once in the tumor microenvironment, neutrophils’ natural properties become greatly distorted, and they become largely responsible for inhibiting T cell activities and allowing more tumor progression. Dysregulation of neutrophils is also associated with many other diseases.
“With the main ketone body depleting neutrophils, it opens the door for investigating the effects of the keto diet and the ketone supplement on diseases ranging from inflammatory bowel disease to arthritis,” Murphy says.
Lu agrees.
“What’s exciting is that we’re getting closer to the mechanism, backed up by genetic models and what we’re seeing in the tumors themselves, of why this works,” he says.
The American Institute for Cancer Research, the National Institutes of Health and a core facility grant from Indiana Clinical and Translational Sciences Institute funded the work. Other support included the Department of Defense and the Boler Family Foundation at the University of Notre Dame. A provisional patent application has been filed based on this study by the IDEA Center at Notre Dame.
Source: Deanna Csomo Ferrell for University of Notre Dame