New research in cells finds that the PFAS chemical GenX suppresses the neutrophil respiratory burst—the method white blood cells known as neutrophils use to kill invading pathogens.
The study is an important first step in understanding how both legacy and emerging PFAS chemicals might affect the body’s innate immune system.
PFAS are a class of per- and polyfluoroalkyl chemicals used to make consumer and industrial products more resistant to water, stains, and grease. According to the US Environmental Protection Agency, there are more than 12,000 known PFAS, which also include fluoroethers such as GenX.
“It’s pretty well-established that PFAS are toxic to the adaptive immune system, but there hasn’t been as much research done on their effects on the innate immune system,” says Drake Phelps, a former PhD student at North Carolina State University and first author of the study.
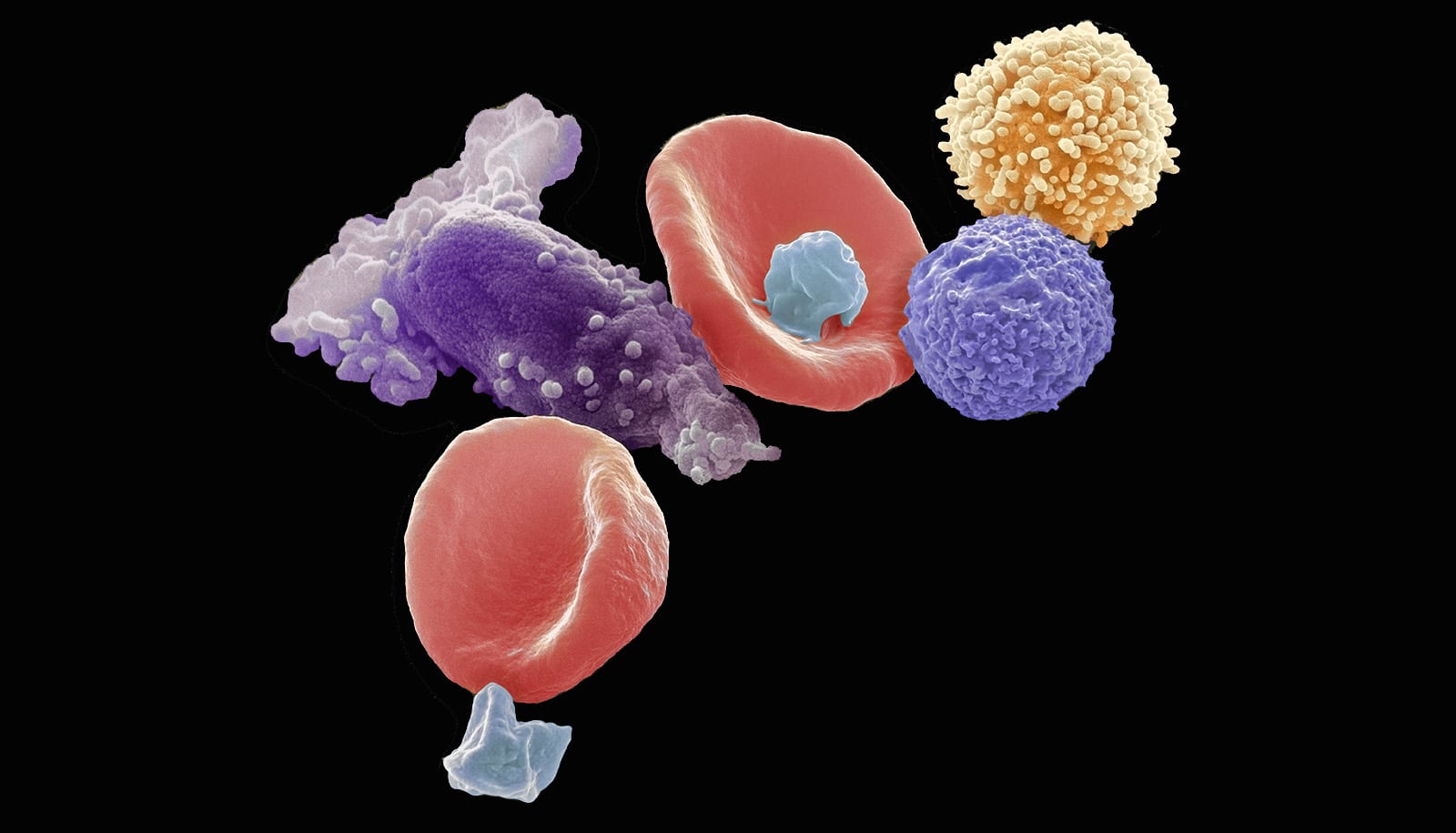
The human immune system has two branches: adaptive and innate. The adaptive branch contains T cells and B cells that “remember” pathogens the body has encountered, but it is slow to mount a defense, acting days—sometimes weeks—after it detects a pathogen.
The innate immune system serves as the body’s first responders, and contains white blood cells that can be dispatched to the site of an invasion within hours. These white blood cells include neutrophils, which can dump reactive oxygen species—think tiny amounts of bleach or hydrogen peroxide that neutrophils manufacture inside their cells—directly onto pathogens, killing them. That process is called the respiratory burst.
Drake and the research team looked at the effect of nine environmentally relevant legacy and emerging PFAS on neutrophils from zebrafish embryos, neutrophil-like cells (cells that can be chemically treated to behave like neutrophils), and human neutrophil cells cultured from donor blood.
Emerging PFAS are chemicals, like GenX, developed to replace older, legacy PFAS that had proven toxic. All of the PFAS included in this study were detected in both the Cape Fear River in North Carolina and the blood serum of residents whose drinking water came from the Cape Fear River.
The embryos and cells were exposed to 80 micromolar solutions of each chemical:
perfluorooctanoic acid (PFOA), perfluorooctane sulfonic acid potassium salt (PFOS-K), perfluorononanoic acid (PFNA), perfluorohexanoic acid (PFHxA), perfluorohexane sulfonic acid (PFHxS), perfluorobutane sulfonic acid (PFBS), ammonium perfluoro(2-methyl-3-oxahexanoate) (GenX), 7H-perfluoro-4-methyl-3,6-dioxa-octane sulfonic acid (Nafion byproduct 2), and perfluoromethoxyacetic acid sodium salt (PFMOAA-Na).
Of the nine PFAS tested, only GenX suppressed the neutrophil respiratory burst in embryonic zebrafish, neutrophil-like cells, and human neutrophils. PFHxA also suppressed the respiratory burst, but only in embryonic zebrafish and neutrophil-like cells.
The researchers caution that while the results of this preliminary study are interesting, they raise more questions than they answer.
“The longest chemical exposure in our study was four days, so obviously we can’t compare that to real human exposure of four decades,” says Jeff Yoder, professor of comparative immunology and corresponding author of the work. “We looked at a high dose of single PFAS over a short period, whereas people in the Cape Fear River basin were exposed to a mixture of PFAS—a low dose over a long period.
“So while we can say that we see a toxic effect from a high dose in the cell lines, we can’t yet say what effects long-term exposure may ultimately have on the immune system. This paper isn’t the end of the road—it’s the first step. Hopefully our work may help prioritize further study of these two chemicals.”
The study appears in the Journal of Immunotoxicology and had support from the National Institute of Environmental Health Sciences (NIEHS), the North Carolina State University Center for Environmental and Health Effects of PFAS, and the North Carolina State University Center for Human Health and the Environment (CHHE). Jamie DeWitt, professor of pharmacology and toxicology at East Carolina University, is coauthor.
Source: NC State