Scientists have discovered a way that brain cells protect themselves from protein aggregates in mice.
The discovery could lead to new treatments for Parkinson’s and other neurodegenerative diseases.
These protein clumps in the nerve cells of the brain can travel from nerve cell to nerve cell, causing neurodegenerative diseases to progress.
Individual, non-aggregated alpha-synuclein proteins play a key role in the release of the neurotransmitter dopamine in nerve cell synapses and are important to the functioning of a healthy brain. But large numbers of alpha-synuclein molecules may aggregate on long microscopic fibers, or fibrils. When that happens, nerves can no longer carry out normal function.
Further, the fibrils are toxic to the nerve cells so dopamine-producing cells die, leaving the brain undersupplied with dopamine. This leads to typical Parkinson’s clinical symptoms such as muscle tremors, researchers say.
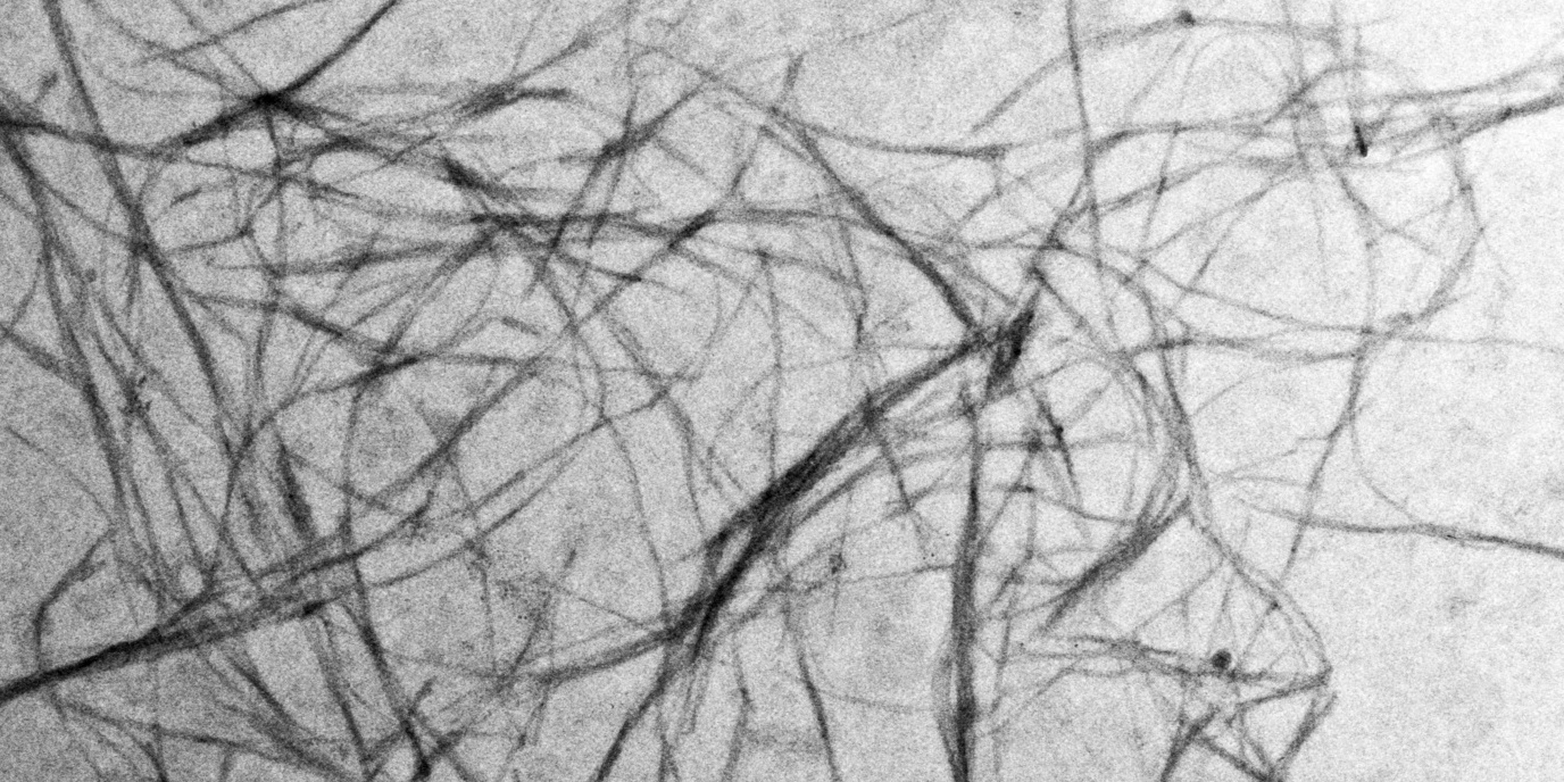
Using cell culture experiments, the researchers showed that it is the alpha-synuclein fibrils that can enter healthy cells and accumulate.
“Once the fibrils enter a new cell, they ‘recruit’ other alpha-synuclein molecules there, which then change their shape and aggregate together. This is how the fibrils are thought to infect cells one by one and, over time, take over entire regions of the brain,” says Paola Picotti, professor of the biology of protein networks at ETH Zurich.
As reported in Science Translational Medicine, researchers discovered a cellular mechanism that breaks down alpha-synuclein fibrils naturally. A protein complex called SCF detects the alpha-synuclein fibrils specifically and targets them to a known cellular breakdown mechanism.
In a test with mice, the researchers showed how this blocks the spread of fibrils. When the researchers switched off SCF’s function, the alpha-synuclein fibrils no longer cleared up in the nerve cells—and instead accumulated in the cells and spread throughout the brain.
Picotti and lead author Juan Gerez, a former postdoc in her group, say they see promising opportunities in how they could apply this SCF breakdown mechanism in therapy.
“The more active the SCF complex, the more the alpha-synuclein fibrils are cleared, which could slow down or eventually stop the progression of such neurodegenerative diseases,” Gerez says.
The short-lived SCF complex dissipates within minutes. Therapeutic approaches would focus on stabilizing the complex and increasing its ability to interact with alpha-synuclein fibrils.
Transplanting nerve stem cells into patients’ brains could offer another treatment approach, Picotti says. Previous attempts haven’t been very successful because the alpha-synuclein fibrils in the brain infected the healthy cells, she says.
“If we can manage to modify the stem cells in such a way that they either don’t let fibrils in or that they immediately break down any fibrils they do let in, this could progress stem cell therapy,” she says. Finally, gene therapy could stabilize the SCF complex in nerve cells and increase its activity.
“However, when it comes to potential therapies, we’re still right at the beginning,” Gerez says. “Whether effective therapies can be developed is still unclear.”
Additional researchers are from ETH Zurich, University Hospital Zurich, and the University of California San Diego.
Source: ETH Zurich



