Researchers have learned more about how the parasitic protozoa that cause malaria hijack human red blood cells.
The parasites that cause malaria symptoms in humans enter the red blood cells of a host and quickly rearrange things to their liking by inserting their own proteins. But, until now, how those proteins pass into the host cell hasn’t been clear.
Liver first
Josh Beck, an assistant professor of biomedical sciences at the Iowa State University College of Veterinary Medicine, says the newfound understanding of how the parasites take charge of red blood cells could help medical researchers discover better treatments for malaria, a disease that kills nearly half a million people per year, mostly in tropical and subtropical regions.
The protozoa that causes malaria enter the human body via the bite of an infected mosquito. The parasites initially develop in liver cells before moving into a host’s red blood cells, which is when the symptoms of the disease arise.
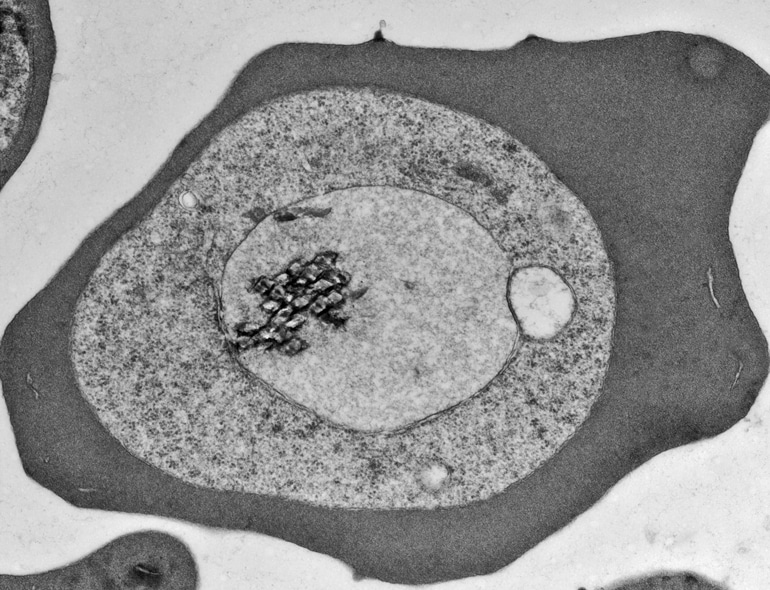
A vacuolar membrane covers the parasites, and they must pass proteins through it in order to make changes to the red blood cell that allow them to survive and avoid the host immune response.
The new research, which appears in Nature and Nature Microbiology, helps to map the mechanism that parasites use to transfer the proteins and other molecules through the membrane.
“Malaria parasites survive in human red blood cells,” says Beck. “To do so, they dramatically change the red blood cell to create a happy home for themselves.”
Dual function
To pass through the membrane the proteins need to be unfolded and then threaded through a small channel, like unwinding a ball of string to pass it through the eye of a needle. The Plasmodium translocon of exported proteins, or PTEX for short, which is a molecular machine complex composed of three parasite proteins, performs this process, Beck says.
One of these proteins does the unfolding while another forms the channel. The third component connects the other two.
Researchers found this same channel through the membrane also serves an unexpected second function, providing a pathway for smaller molecules, such as waste and nutrients, to pass in and out of the parasite. That dual function means the pathway plays an especially critical role for the parasite, making it a potential target for new therapies, Beck says.
“Understanding the structure and function of PTEX can give us clues about how to design new drugs. It’s a weak point that could be exploited. Inhibiting that pathway would be disastrous for the parasite.”
Source: Iowa State University



