Along with the 0-10 rating scale, asking the question “Is your pain tolerable?” could help doctors decide if treatments, including opioid medications, are actually necessary, research shows.
“Because of concerns about overtreatment of pain with opioids there has been an enormous effort to rethink how we ask patients about pain,” says John D. Markman, director of the Translational Pain Research Program in the University of Rochester Medical Center department of neurosurgery and lead author of the paper in JAMA Network.
The findings show that almost 4 out of 5 patients in the primary care setting who rated their pain as “moderate” in intensity found it tolerable and as many as 30 and 40% of people who rated their pain as “severe” (a score of 7 or more) also described the pain as “tolerable.”
“Knowing that patients consider their pain to be tolerable, physicians wouldn’t necessarily prescribe a medication with serious risks or expose them to surgery,” Markman says. Instead, it could be an opening for a clinician to explore mood, sleep disruption, or the curtailing of certain activities to control pain.
The study asked 537 patients at 157 primary care practices in the Western New York region to rate their chronic pain using the 0-10 numeric rating scale (NRS) and also respond yes or no to the question: “Is your pain tolerable?”
Researchers conducted the study in collaboration with the Greater Rochester Practice-Based Research Network (GR-PBRN), a diverse group of primary care practices that collaborates with researchers to ask and answer clinical and organizational questions central to primary care representing 350,000 patients.
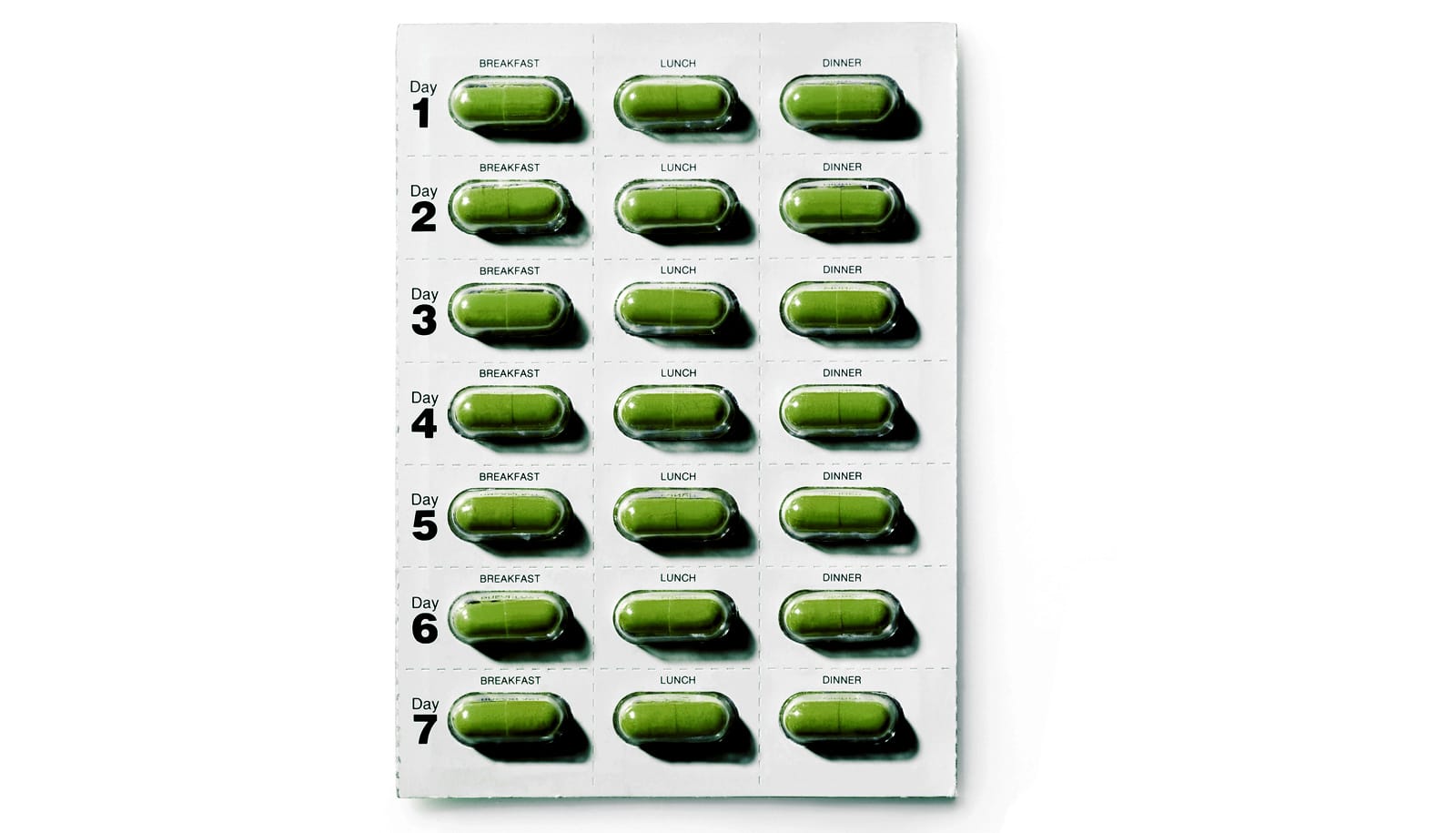
The 0-10 NRS—used tens of millions of times per day in the US healthcare system—is integral to:
- Health payment systems overseen by the Joint Commission (JCO), the accrediting organization for all hospital and outpatient facilities in the United States.
- Food and Drug Administration (FDA) approval and regulation of products that treat pain.
- Pain studies conducted by the National Institutes of Health (NIH).
The numeric ratings are “very good at detecting change from one moment to another in an individual patient,” for example as the patient recovers in a hospital after surgery, Markman says. But they may have “very little relevance” when patients who have lived with chronic pain for several years visit their doctors for periodic checkups.
“If, instead, a patient could say ‘my pain is tolerable when I’m doing this but intolerable when I’m doing that,’ and it’s in the context of that patient’s life, I frankly think that’s much more useful, and is what doctors really want to know,” Markman says.
Markman says he is encouraged by the “very aggressive search going on to validate alternatives to the numerical rating scale that focus on high impact pain.”
“In order to transform how we treat pain to make treatments safer and more effective, we need to start with a reformation in how we ask patients about pain,” he says. “This paper is one attempt to do that.”
Markman has received consulting fees and research funding support from Pfizer, which funded this investigator-initiated study, but the company was not involved in its design, collection of data, interpretation, or its publication.
Source: University of Rochester