A new handheld device called CLiKX could improve the current surgical treatment of otitis media with effusion, also called “glue ear,” in children.
OME is the leading cause of hearing loss and visits to the doctor among children worldwide.
OME is a condition in which fluid, instead of air, fills the middle ear. If left untreated, it can cause a series of life-altering complications such as hearing impairment, middle ear bone erosion or tumor, and brain infection. OME has also been shown to cause delays in the speech, language, and academic abilities of young children.
Specially designed to improve on the surgical treatment of OME, CLiKX comes from a team led by associate professor Tan Kok Kiong from the department of electrical and computer engineering at the National University of Singapore Faculty of Engineering.
“The first line therapy for OME is usually the prescription of antibiotics and treatment of blocked ear tubes. But sometimes, the antibiotics may not be effective against OME,” explains team member Lynne Lim, adjunct associate professor in the department of otolaryngology at the NUS Yong Loo Lin School of Medicine and senior ear nose and throat consultant at Mount Elizabeth Medical Centre.
“For patients with three or more episodes of OME within a year—especially if there is hearing loss and speech difficulties, some with craniofacial predispositions, or those who are concerned about building resistance to long term use of antibiotics, grommet tube placement surgery is currently the gold standard of care.
“A grommet is a very small tube that is inserted onto the patient’s ear drum during surgery to help drain away fluid in the middle ear. Each procedure usually takes about 30 minutes under general anesthesia to complete,” explains Lim.
“CLiKX can potentially shift the current standard surgical procedures for OME,” says Tan. “With this pistol-like applicator, the grommet tube can be easily inserted into a patient’s ear within a single click. In less than a second, the procedure is done.
“This simple procedure has the potential to be administered in a doctor’s consultation room under local anesthesia, or out of the operating theatre under intravenous conscious sedation without general anesthesia. Preoperative preparation and postoperative recovery time for patients are significantly reduced. At the same time, risks of general anesthesia are avoided.
“We expect costs, manpower, and resources to be lowered substantially, and this in turn, would be welcomed by patients, healthcare institutions, and insurers.”
Ear infections really do require 10 days of antibiotics
Grommet tube placement surgery involves making a cut on the eardrum, and placing a tiny ventilation tube, called a grommet, through the hole to drain the ear fluid. The surgery involves a large healthcare team, costly surgical equipment, and set-up in the operating theatre, which is an economic burden not only to patients, but also to hospitals and healthcare insurers.
The palm-sized CLiKX can deliver the grommet tube into a patient’s ear quickly and safely using a sensor-controlled automation process. This minimizes the overall contact time with the patient’s eardrum and prevents over-deformation and excessive pressure, thereby reducing discomfort and trauma for the patients.
In the long term, are ear tubes worth the risk?
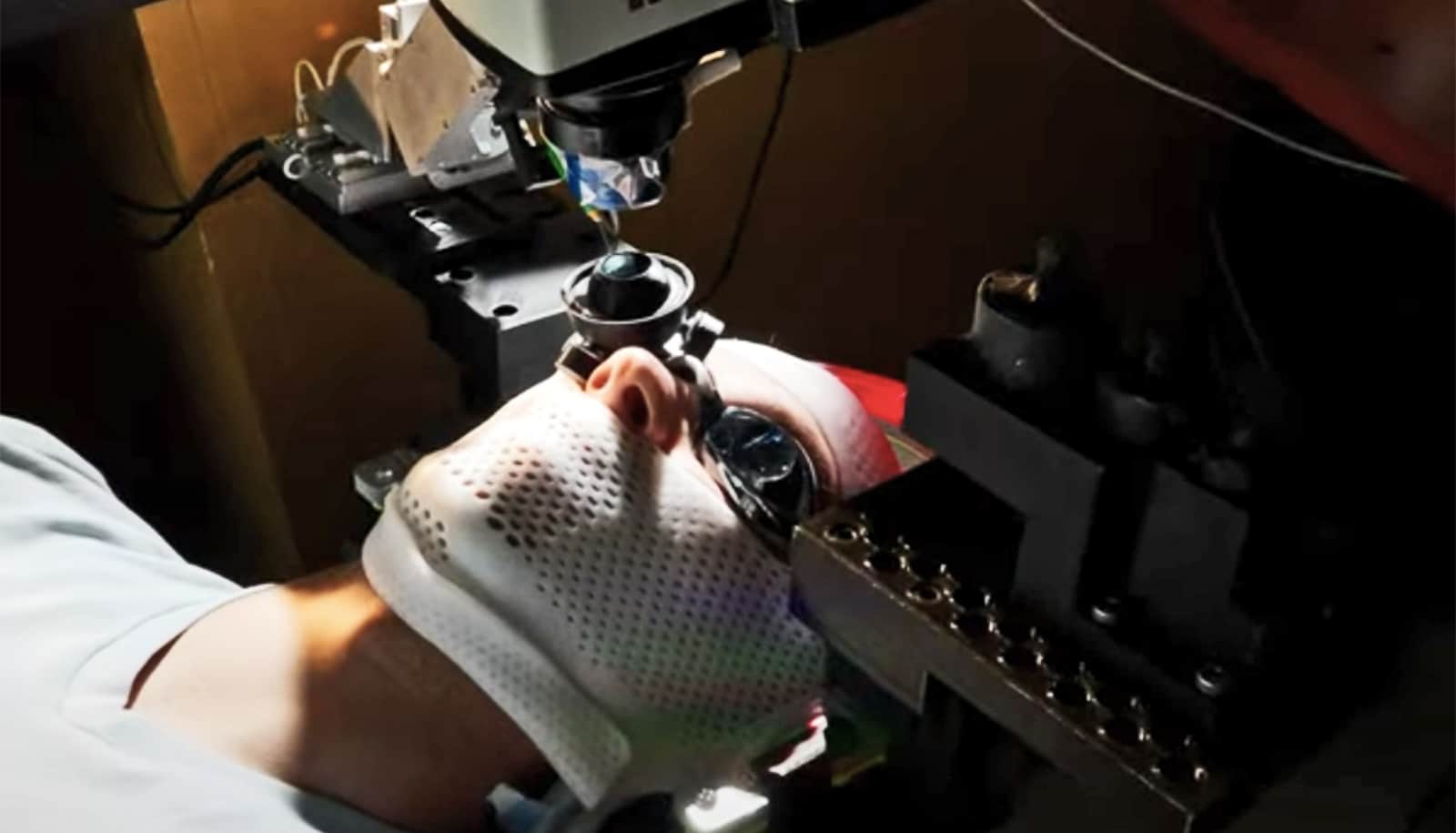
To carry out the procedure, surgeons can potentially use a simple eye-loupe that does not require bulky and costly surgical microscopes. The 185-gram CLiKX also works well with a range of commercially available grommets and does not require any custom-made grommet tubes. In addition, the procedure using CLiKX would potentially require only light or moderate sedation or local anesthetic.
“In many underdeveloped areas where proper healthcare infrastructure and general anesthesia are not always available, many patients with OME do not have access to treatment in a timely manner,” says Lim. “Some of these patients have to live with the condition, its associated hearing loss and complications. CLiKX can make a significant impact by making grommet placement surgeries more accessible to these patients most in need, and it simplifies the procedure for doctors and patients.”
Building on the promising results from the earlier phases of the project, the NUS team aims to conduct the trial in humans in Singapore in 2018. The team is keen to work with partners to further develop and commercialize the device, and they aim to launch the device in the market by 2020.
Source: National University of Singapore