People living in the most populous, low-income areas in New Jersey with the highest risk for opioid overdoses have less access to the potentially life-saving opioid reversal drug naloxone, according to a new study.
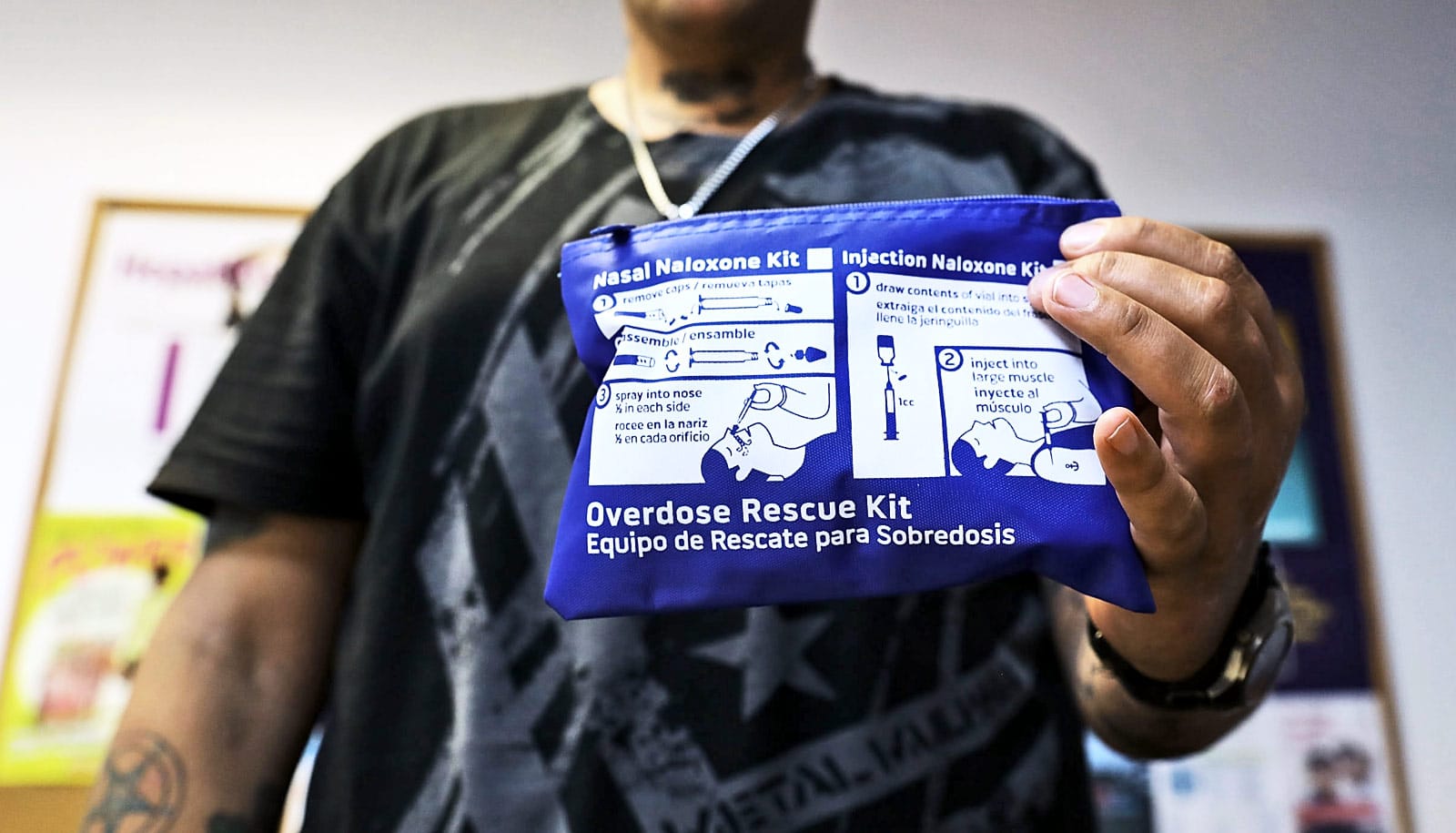
Researchers analyzed how a city’s population and affluence correlate with the availability of naloxone in retail pharmacies. Also known by the brand names Narcan and Evzio, naloxone reverses the effects of opioids on the central nervous system in an overdose. Unfortunately, it’s also expensive and difficult to obtain.
“This shows that New Jersey has naloxone ‘deserts’ where the medication is needed most.”
New Jersey’s opioid-related death rates are among the fastest growing in the nation, rising 29 percent from 1,376 deaths in 2016 to 1,969 deaths in 2017, according to the Centers for Disease Control and Prevention.
“Naloxone can be a life-saving drug in the hands of bystanders,” says Lewis Nelson, chair of the emergency medicine department at Rutgers New Jersey Medical School. “Although retail pharmacies in New Jersey are permitted to dispense naloxone without a prescription, not all do.”
The study, which appears in the Journal of Medical Toxicology, compared naloxone availability in 90 retail pharmacies in 10 New Jersey cities to median household income, population, and the prevalence of opioid-related hospital visits over a five-month period.
Naloxone was available in 60 percent to 70 percent of retail pharmacies in more affluent, lower-population communities, but was available in less than 25 percent of lower-income, high-population cities, the study shows.
“These cities with limited naloxone access also have the most severe opioid-related public health concerns,” says lead author Kevin Lozo, a medical student at Rutgers New Jersey Medical School. “This shows that New Jersey has naloxone ‘deserts’ where the medication is needed most.”
Two possible explanations may account for the disparities: lack of insurance and types of retail pharmacies in low-income areas, Lozo says. “Cities with an underinsured population do not create demand for pharmacies to stock naloxone, which can cost up to thousands of dollars.”
Also, pharmacy retail chains CVS and Walgreens have committed to stocking naloxone in their stores, but few of them are located in low-income cities.
“We found that 75 percent of the CVS and Walgreens stores surveyed had naloxone available versus only 14 percent of other retailers,” says Diane Calello, executive and medical director of New Jersey Poison Control based at the medical school and senior author of the study.
“This study demonstrates that there is much more to be done to get naloxone into the hands of people who most need it.”
Source: Rutgers University