Six months into the pandemic, more than 20% of nursing homes still report severe shortages of staff and personal protective equipment, a new study shows.
Nursing home residents account for nearly half of all COVID-19 deaths in the US. Age, chronic medical conditions, and congregate living quarters place these residents and their caregivers at high risk of contracting the disease.
“Twenty percent is a lot, given where we are in the course of this pandemic. I would have hoped by month six we would be close to 0%,” says Brian E. McGarry, assistant professor of geriatrics/aging and public health sciences at the University of Rochester Medical Center and lead author of the paper, published as a fast track ahead of a print article in the journal Health Affairs.
“While there has been some shifting in which nursing homes have been reporting these problems, from a national level, we’re still not on the right trajectory.”
The study is among the first to report results from a new Centers for Medicare and Medicaid Services (CMS) COVID-19 Nursing Home Database, which includes responses from more than 15,000 nursing homes and other long-term care facilities—or 98% of the US total—regarding the impact of COVID-19 on staff and residents.
The database is far from perfect, McGarry says. Some of the questions nursing homes respond to are “ambiguous” and could be honed to elicit more details.
Nonetheless, based on nursing home responses submitted for the database from May 18 to June 14, and from June 24 to July 19, the researchers determined that:
- Rates of both staff and personal protective equipment (PPE) shortages did not meaningfully improve from May to July.
- The facilities most likely to report shortages were those with COVID-19 cases among residents and staff, those serving a high proportion of Medicaid recipients, and those that score lower on a five-star quality rating system used by CMS.
“Having a shortage of any type of staff affects every aspect of clinical care, whereas a shortage of any PPE element can break infection control protocols,” the study says.
N95 masks and gowns continue to top the list for the most commonly reported PPE shortages, with gown shortages easing slightly as of July 19. Though the federal government promised in May to provide nursing homes with a two-week supply of PPE, “many nursing homes reported that they did not receive adequate PPE through this initiative.”
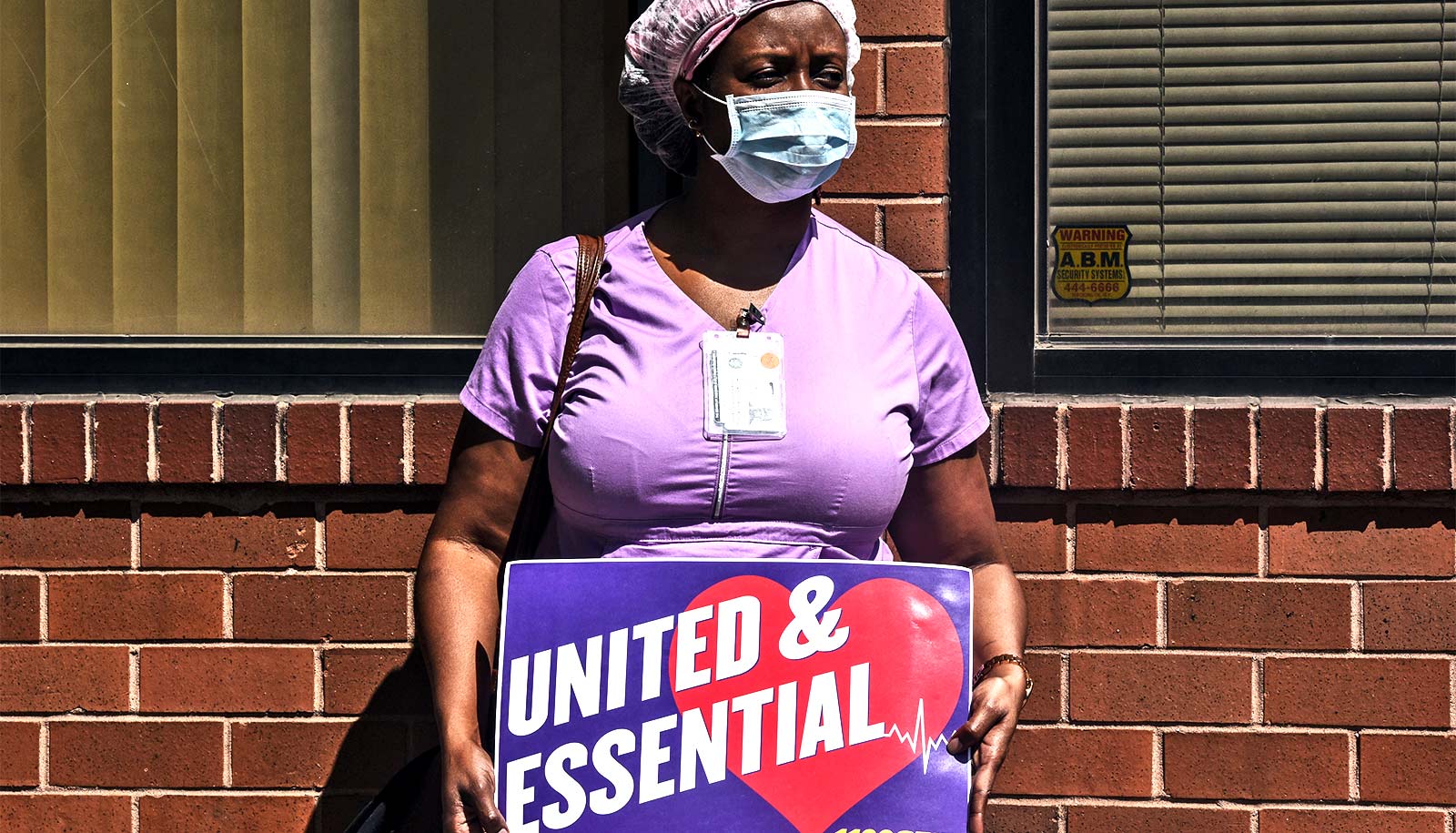
And although the Centers for Disease Control called for nursing homes to develop plans to mitigate staffing shortages, “many nursing homes struggled with staffing prior to COVID-19, and shortages have reportedly been magnified because many staff are unable or unwilling to work in these conditions,” the study reports. Nurses, nursing aides, and “other staff” continued to be staff categories with the most shortages.
“It is concerning, although not unexpected, that more disadvantaged and lower quality nursing homes, such as those with a higher percent of revenue from Medicaid or those with lower star ratings, have worse staff shortages. These are the facilities whose profit margins will be necessarily lower due to the underpayment of Medicaid for nursing home costs,” the study says.
“This is not just about bad nursing homes doing a bad job,” McGarry says. “Nursing homes are very much at the mercy of the levels of infection in the communities around them. COVID-19 is indiscriminate. It doesn’t care whether you’re a five-star facility or not. The most effective way to prevent COVID-19 outbreaks in nursing homes is reducing the prevalence of the disease in the communities they serve.”
In addition, the researchers recommend that:
- Top priority be put on insuring that all nursing homes have a minimally sufficient supply of PPE “if policymakers intend to save as many lives as possible.”
- Future stimulus packages provide additional, targeted financial support for direct patient care and supplies in nursing homes with more disadvantaged populations, coupled with appropriate oversight to ensure funds are used appropriately.
- States with the severest shortages of nursing home staff “prioritize their nursing homes’ resilience” to deal with outbreaks.
- Medicare continue its commitment to gathering and disseminating information on nursing homes’ available resources, but also update survey questions to reflect current realities of the pandemic, including testing turnaround time.
Additional coauthors are from Harvard Medical School.
Source: University of Rochester