An increase in nightmares and hallucinations could signal the onset of autoimmune diseases, such as lupus, according to a new study.
These neuropsychiatric symptoms can also act as early warning signs and help people with lupus potentially identify a coming flare when their disease worsens for a period.
“Many people don’t know that neuropsychiatric symptoms, including confusion, hallucinations, and vivid nightmares, can be part of autoimmune diseases like lupus,” says James Alan Bourgeois, a professor in the psychiatry and behavioral sciences department at the University of California, Davis, and coauthor of the study in eClinicalMedicine.
“If someone presents with new psychotic symptoms and has other autoimmune symptoms, and a family history of autoimmune disease, a provider is advised to clinically evaluate him or her for lupus before assuming a patient has schizophrenia or other primary psychotic disorder.”
“It’s important that clinicians talk to their patients about these types of symptoms and spend time writing down each patient’s individual progression of symptoms,” says lead author Melanie Sloan, a researcher in the public health and primary care department at the University of Cambridge.
“Patients often know which symptoms are a bad sign that their disease is about to flare, but both patients and doctors can be reluctant to discuss mental health and neurological symptoms, particularly if they don’t realize that these can be a part of autoimmune diseases.”
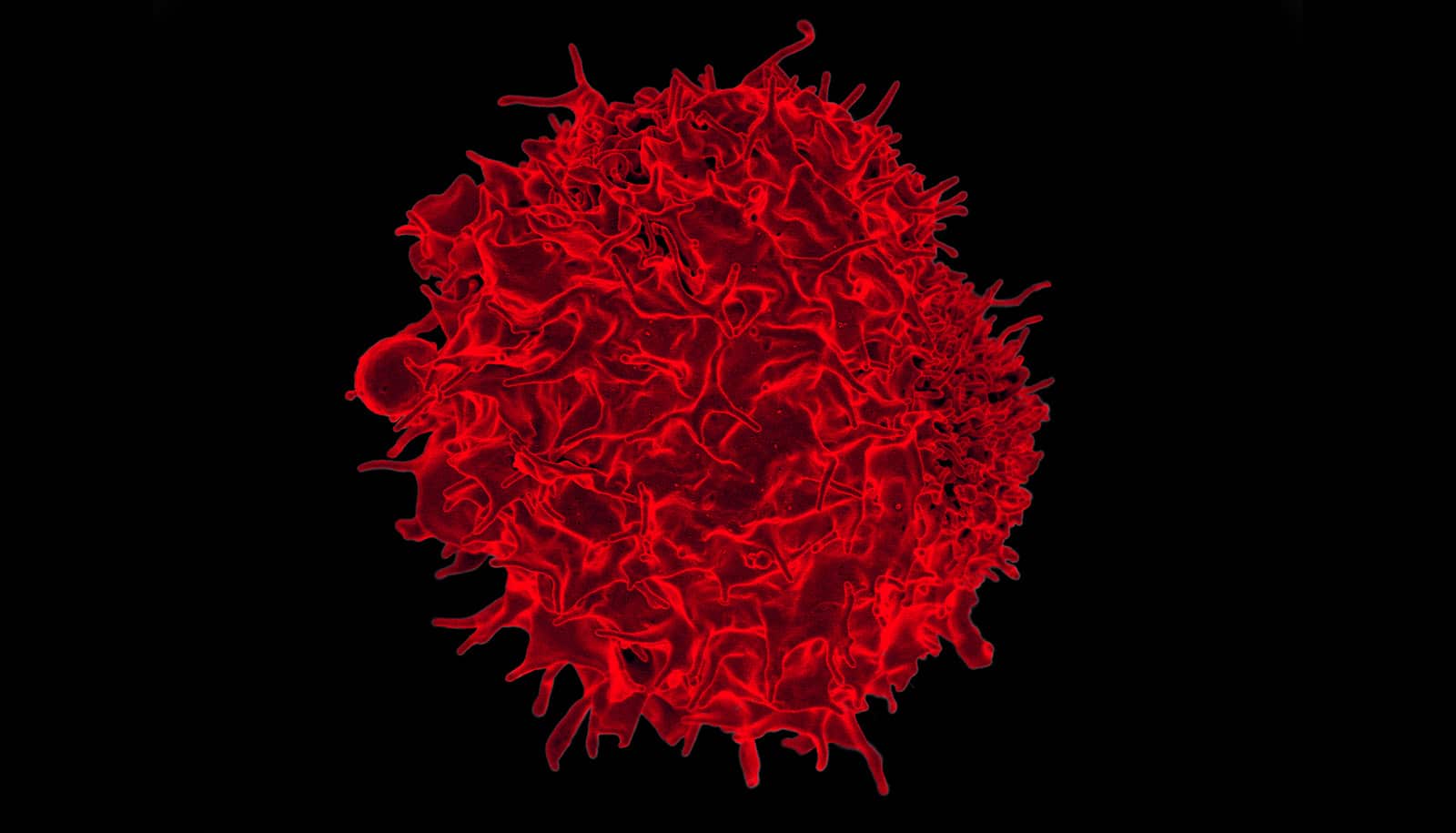
Lupus, formally known as systemic lupus erythematosus (SLE), is an autoimmune inflammatory disease known for its effect on many organs, including the brain. According to the Lupus Foundation of America, about 1.5 million people in the US have lupus, and an estimated 5 million globally. The majority of those with lupus—nine out of 10—are people who were designated female at birth.
The researchers surveyed 676 people living with lupus and 400 clinicians. They also conducted detailed interviews with 69 people living with systemic autoimmune rheumatic diseases (including lupus) and 50 clinicians.
In the study, the team asked patients about the timing of 29 neuropsychiatric symptoms (such as depression, hallucinations, and loss of balance). In interviews, patients were also asked if they could list the order of symptoms that usually occurred when their disease was flaring.
One of the more common symptoms reported was disrupted dream sleep, experienced by three in five patients, a third of whom reported this symptom appearing over a year before the onset of lupus.
Just under one in four patients reported hallucinations, although for 85% of these, the symptoms did not appear until around the onset of the disease or later.
When the researchers interviewed the patients, however, they found three in five lupus patients and one in three with other rheumatology-related conditions reported increasingly disrupted dreaming sleep just before their hallucinations. These nightmares were often vivid and distressing, involving being attacked, trapped, crushed, or falling.
The study interviewers found that using the term “daymares” to talk about hallucinations often led to a “lightbulb moment” for patients, and they felt that it was a less frightening and stigmatized word.
Patients experiencing hallucinations were reluctant to share their experiences. Many specialists said they had never considered nightmares and hallucinations as being related to disease flares.
“For many years, I have discussed nightmares with my lupus patients and thought that there was a link with their disease activity,” says senior author David D’Cruz, a professor at King’s College London.
“This research provides evidence of this, and we are strongly encouraging more doctors to ask about nightmares and other neuropsychiatric symptoms—thought to be unusual, but actually very common in systemic autoimmunity—to help us detect disease flares earlier.”
The importance of recognizing these symptoms was highlighted by reports that some patients had initially been misdiagnosed or even hospitalized with a psychotic episode or suicidal ideation, which was only later found to be the first sign of their autoimmune disease.
The UK-registered charity The Lupus Trust funded the work.
Source: UC Davis