Monkeypox, a smallpox-related virus endemic to parts of Central and West Africa, has now emerged in 74 countries, with nearly 2,900 confirmed cases in the US.
The growing number prompted the World Health Organization (WHO) to declare monkeypox a global health emergency, as it did for COVID-19 in 2020.
With more than 16,800 cases globally, some scientists are calling the monkeypox outbreak a pandemic, albeit with a far lower mortality rate than the COVID-19 pandemic.
The disease often starts with fever, chills, headache, fatigue, muscle aches, and swollen lymph nodes—symptoms similar to those of many other illnesses. But monkeypox is marked by raised, pus-filled blisters that dot the skin and is transmitted through direct exposure to the rash, scabs, or bodily fluids, including respiratory droplets.
It is also transmitted by close physical contact with items that touched the rash and are contaminated with virus, such as clothing and bedding.
“This is a known disease presenting in places where it’s not usually found, and in a way that was not immediately raising suspicion for monkeypox,” says Felicia Nutter, assistant professor at Cummings School of Veterinary Medicine at Tufts University who specializes in wildlife health and infectious disease ecology and zoonoses.
“There has been testing and diagnosis, and also activation of public health measures to be able to access vaccine stockpiles. We need much more widespread testing and vaccination to address this disease.”
Nutter has worked as a wildlife veterinarian in Rwanda, Uganda, and the Democratic Republic of Congo and is currently part of the STOP Spillover project with the United States Agency for International Development (USAID).
Here, she explains what you should know about the current monkeypox outbreak, including how it’s transmitted and who is at risk:
How does this outbreak differ from past monkeypox outbreaks?
Monkeypox is usually found in multiple countries in Central and West Africa, where it is transmitted from the natural wildlife hosts (likely rodents) to humans. There is diagnosis and tracking of annual cases in those countries that could number in the hundreds. Because of travel between those countries and others, monkeypox sporadically shows up in places where it is not usually found. Usually, there have been single cases diagnosed because somebody was exposed to monkeypox in a country where it’s normally found then traveled to a country where being diagnosed is not typical.
What’s different about this outbreak is that there has been sustained community transmission of the disease before it was diagnosed. Also, this specific monkeypox virus appears to be from the group known to be less severe, the West African clade, and has a lower case fatality rate than the more severe Central African clade monkeypox.
The way that it’s showing up is also not the classical description of monkeypox. There aren’t a lot of lesions, but rather a few scattered lesions.
Who is most at risk for contracting the virus?
It is important to know that anyone can be infected with monkeypox. If you’re in contact with someone who has been diagnosed with monkeypox, you’re at risk. It’s a viral disease that spreads through close contact. So that means being in physical contact with somebody who has the disease or anything they’ve touched for a prolonged period, if they have an active lesion. For example, if you’re doing laundry for someone who has monkeypox, you could be exposed.
Can you explain why rates of infection are so much higher in Europe? England, Spain, and France have a combined five times the number of monkeypox cases as the US.
There are several possible reasons for that difference. Higher case counts could be because that’s where the community transmission first started, and this is what most experts think is happening. Contact tracing has shown what we call point sources, a single event or activity that resulted in the spread to a number of individuals who then went on to spread to additional individuals. That additional spread is what is called the sustained community transmission.
What always comes to mind is that there are higher case counts there compared to other places, but is it being looked for in other places? Is there an index of suspicion? Are people testing for it in other places or have they not started testing adequately? The WHO, CDC, other public health agencies, and news media are raising awareness, and we all need to pay attention and do our part.
How does testing for monkeypox work?
It isn’t something that’s done in an urgent care clinic. And there’s no rapid test, like the one available for COVID-19, where you get the results in 15 minutes. This is a PCR test done in a referral lab, so samples are collected and sent off for testing. In the US, the CDC initially did all the testing, and now several major commercial laboratory companies also are running the tests.
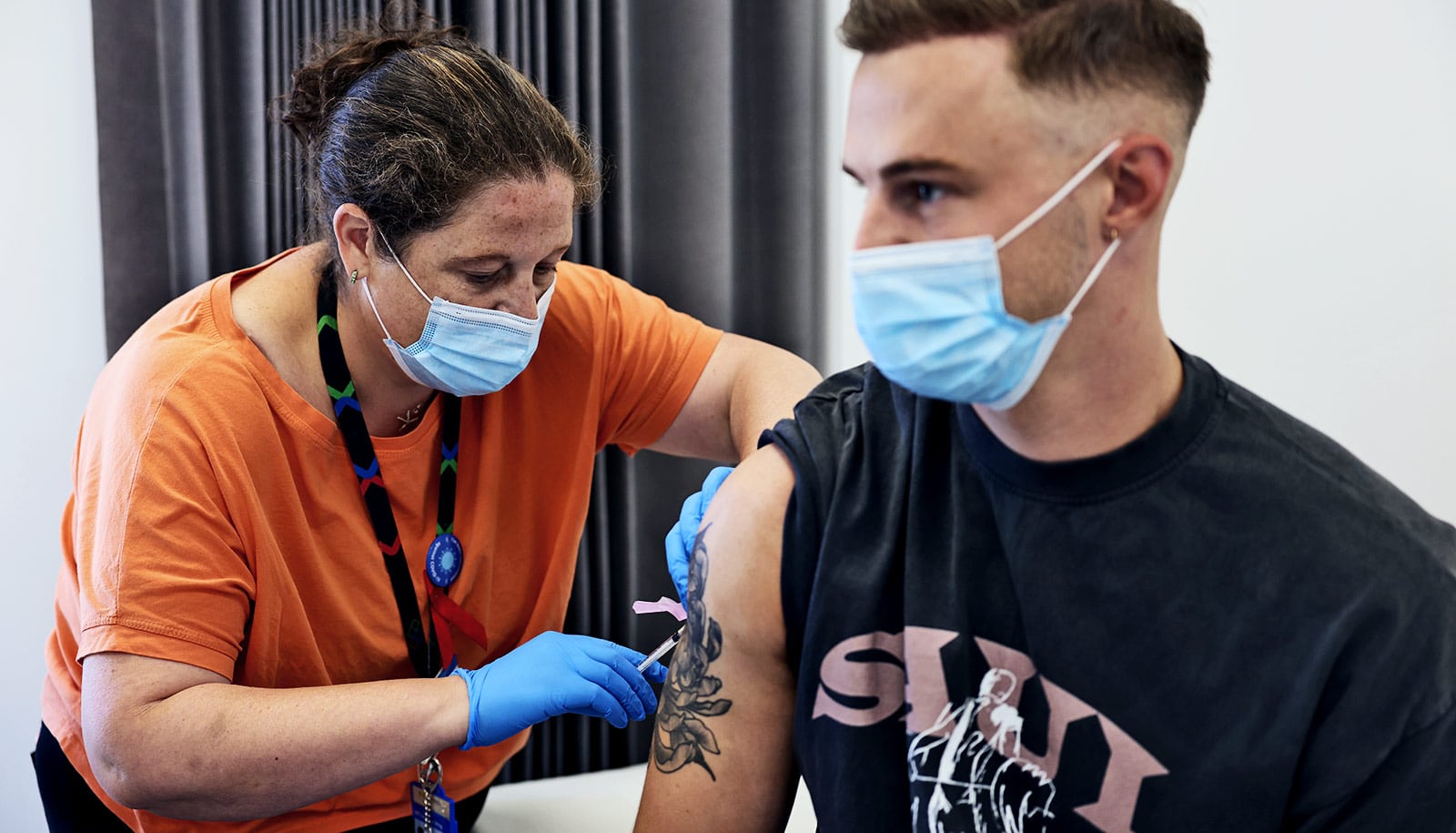
If you know you’ve been exposed, what can a vaccine do?
After exposure, yes, it can be a race between your immune system’s response to the vaccine and your body being affected by the virus. There are other well-known diseases for which we vaccinate in the face of exposure. Rabies is a classic one. If you’ve been bitten by a rabid animal or a suspected rabid animal, you get what is called post-exposure prophylaxis, and that includes a vaccine. By the time the rabies virus is slowly moving toward your central nervous system, the vaccine and your immune response is usually going to be effective and fight it off.
If you think you have been exposed to monkeypox, it is important to inform your doctor and get tested and possibly vaccinated as soon as possible. A monkeypox vaccine given within four days of exposure has the best chance of preventing disease, but even up to two weeks after exposure it can reduce the severity of the symptoms. It’s also important to follow any instructions from health care providers about self-isolation and other methods to reduce the risk of spreading monkeypox.
Are there any myths about monkeypox that should be dispelled? For example, is monkeypox a sexually transmitted infection?
It’s important to be clear about the difference between how the virus is transmitted and the communities in which it was first detected in this current global outbreak. It is not a sexually transmitted disease like chlamydia or herpes. It’s transmitted by close physical contact, and sex is just one of many ways for close physical contact to happen.
There has been some confusion around sexual transmission, because the disease is primarily showing up in networks of men who have sex with men. There is appropriate concern about stigmatization and marginalization of people who are not getting appropriate care.
It’s shades of HIV and AIDS all over again, and we know we can’t go down that road, because it’s harmful to individuals, communities, and overall public health. It’s critical that we provide the right care to those who need it when they need it. The virus does not discriminate, and we shouldn’t either.
Source: Annie Young for Tufts University