The current monkeypox outbreak is moving faster than any in recent history, but virologist Heather Koehler doesn’t see a reason for the rapid spread in the virus itself.
An expert in virus-host interactions, Koehler is conducting research on the monkeypox strain that is currently circulating, working to understand the virus’ genetics by studying its DNA sequence and protein structures.
“We should not be putting any kind of labels on a disease that is transmitted through contact.”
“There are no new, large mutations that could account for the change in transmission,” says Koehler, assistant professor at Washington State University. “I’m not an epidemiologist; I don’t want to predict how or where we should be vaccinating, but there’s something that’s not lining up.”
Koehler says it could be containment strategies are not being implemented appropriately or vigorously enough, or that infected people are not recognizing the symptoms and seeking treatment in time.
Past outbreaks have been relatively small and quickly contained. This time, however, the virus has spread to more than 16,500 cases as of late July, mostly in countries that historically have not had many reported cases of the virus.
Yet, little has changed in the monkeypox genome, says Koehler. While it’s possible that a small change could be driving the spread, researchers have found no obvious changes that would seem to have this large of an impact. Analysis has shown there are less than 100 out of over 197,000 nucleotides, a type of DNA base pair, that are different in the current virus than the one from a smaller 2017 outbreak in the United Kingdom.
“It’s pretty much the same virus,” she says.
Why the outbreak now?
Koehler studies virus-host interactions at molecular levels. She has been investigating how human proteins interact with the proteins of the currently circulating monkeypox strain which has origins in West Africa.
That region is considered endemic to this monkeypox virus, meaning it has animal species that act as a reservoir for the zoonotic disease that can transfer from animals to humans. It is not uncommon to find cases there. In the past, non-endemic countries saw cases that were linked to travel to endemic countries, non-traditional animal hosts, or human-to-human spread. This current outbreak, Koehler says, appears to be primarily dependent on human-to-human transmission.
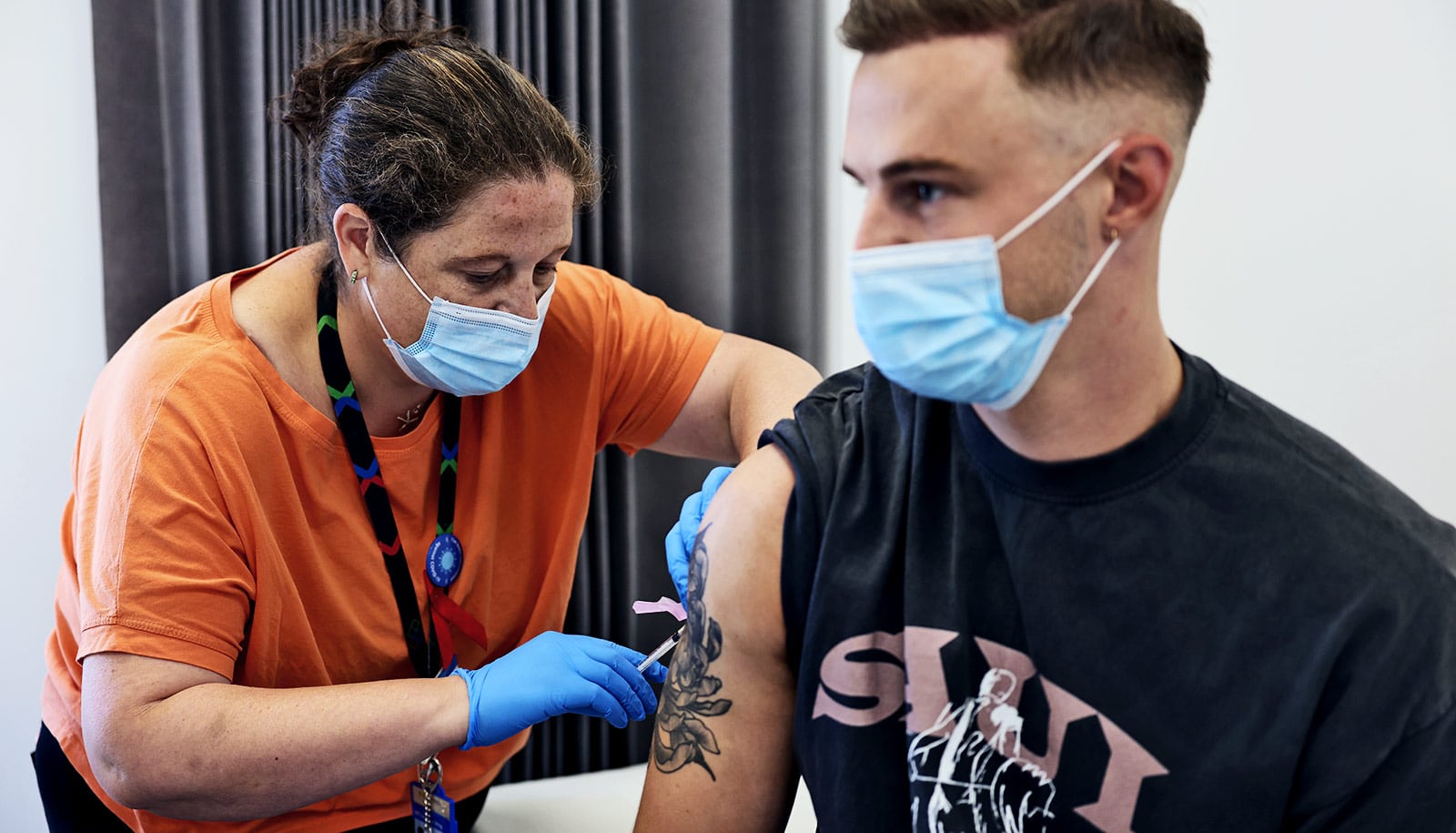
The size of the current outbreak caused the World Health Organization director to overrule a panel of advisers on July 23 to declare monkeypox a global health emergency. On July 28, the White House announced the first phase of a national monkeypox vaccine strategy in the United States. Koehler is glad to see these urgent steps happen.
“This is something that’s spreading faster than any virologist would have predicted based on prior outbreaks that were rapidly contained,” she says. “The widespread nature of this outbreak is unprecedented.”
Monkeypox myths and detection
There have been many situations in the past in which people traveling to endemic regions come back with the disease, but through isolation and vaccination of people’s contacts it was contained. Many countries have stockpiles of the vaccine, including the US Centers for Disease Control and Prevention, which has distributed doses to heavily affected areas, such as King County in Washington state. Yet, the response has not been enough to stop the spread.
One problem could be that people are not identifying as having been exposed to monkeypox, Koehler says. The disease has an incubation period, but people are not usually contagious until symptoms appear. Symptoms include fever, muscle fatigue, and severe headache, but skin lesions are a tell-tale sign of the virus.
“The lesions are pretty characteristic or distinct. It’s not like there’s much room for interpretation,” Koehler says. For instance, monkeypox lesions can appear anywhere on the body including the palms of the hands and the bottoms of the feet—unlike lesions from other diseases such as herpes or chicken pox.
Koehler also fears that misrepresentation of the disease as spreading primarily by men having sex with men is making the problem worse. Monkeypox can be transmitted through any type of close contact including a handshake or a hug. Recently, two cases in children have been identified, a worrying sign because children and pregnant women are among the most vulnerable to the worst effects of the disease.
There is nothing about this virus that targets any particular community, Koehler says, pointing out that viruses sometimes appear in a particular community simply because it is a tight-knit group of people who interact regularly.
Koehler says the way some news outlets are talking about monkeypox is not only biased and inaccurate but also could prevent people from seeking medical attention.
“We should not be putting any kind of labels on a disease that is transmitted through contact,” she says. “It doesn’t matter your sexual orientation; it doesn’t matter what kind of physical engagement you’re having—if you’re having prolonged physical contact with an infected lesion, you have the capacity to pick it up.”
Source: Washington State University