Sub-millimeter microsensors tiny enough to inject under the skin could monitor your health in the future thanks to a new, super-sensitive wireless reader.
The advance is a step toward making tiny under-the-skin implants that continuously measure a person’s blood glucose, heart rate, and other physiological conditions a reality.
Technology limitations have largely hampered current efforts to make these microsensors small. Too small for battery power, the sensors require a reader near them that constantly detects signals such as chemical or pressure changes using magnetic fields.
For a reader to make sense of the signals, the sensor must be large enough to create a strong signal in the reader. So far, researchers have not been able to create viable microsensors below 1 millimeter.
The researchers developed a new way of measuring the signal, by calibrating the wireless reader to work at an exceptional point—a special state where the reader becomes extremely sensitive to nearby objects. The result is that the reader is so sensitive—three times more sensitive than existing readers—that it can even read the tiny signals the sub-millimeter microsensors emits.
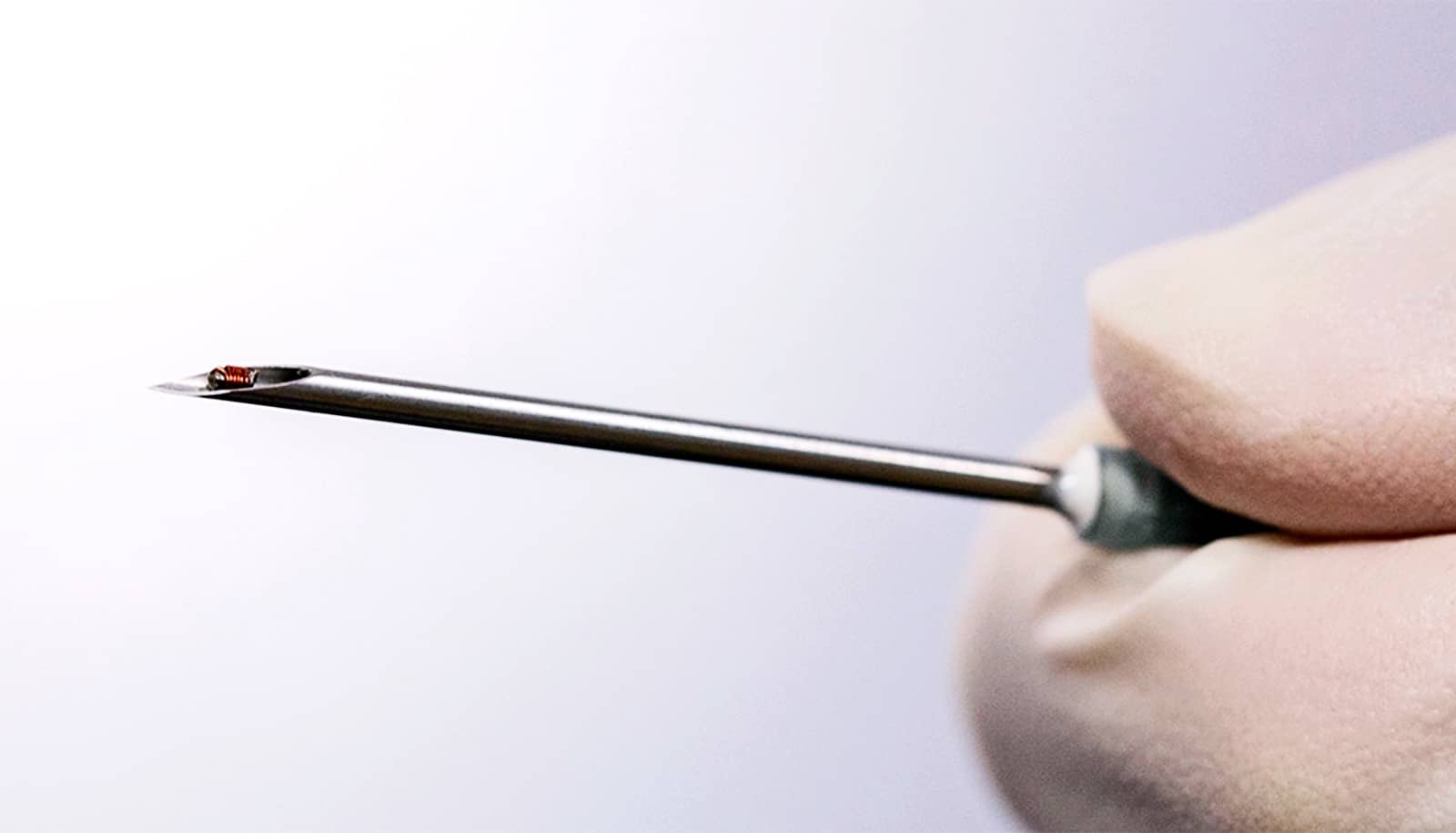
The team developed a working prototype of the reader that can read a microsensor 0.9 millimeters in diameter after it has been injected beneath the skin using a syringe. In lab experiments, the reader successfully monitored the rate of breathing and heart rate by detecting subtle movements of the battery-free microsensor.
“We hope that our breakthrough will be a trailblazer for the future of minimally invasive health monitoring solutions where patients are immediately alerted whenever their physiological conditions such as heart rate and blood glucose cross a critical threshold,” says John Ho, assistant professor at NUS Electrical and Computer Engineering and the NUS Institute for Health Innovation and Technology.
“Now that we have proven the viability of our reader, the next step is to develop a suite of passive (battery-free) microsensors that can monitor various physiological parameters such as glucose, bioelectrical activity, and blood chemistry.”
The study appears in Nature Electronics.
Source: National University of Singapore