A new way to forestall Alzheimer’s disease in a laboratory setting could one day help in devising targeted drugs that prevent it.
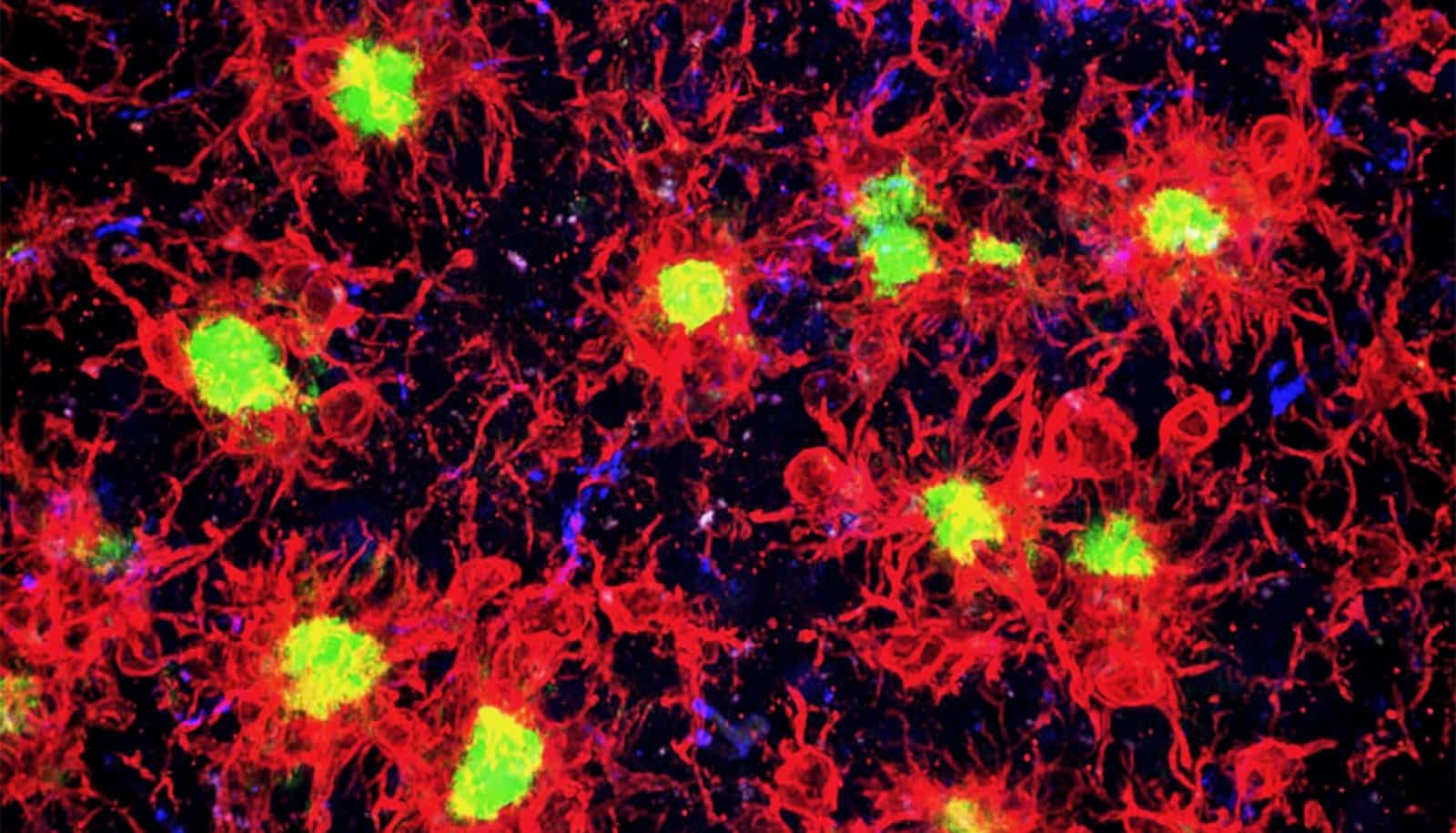
Researchers found that when they removed brain immune cells known as microglia from rodent models of Alzheimer’s disease, beta-amyloid plaques—the hallmark pathology of Alzheimer’s—never formed.
Previous research has shown most Alzheimer’s risk genes are turned on in these immune cells, suggesting they play a role in the disease.
“However, we hadn’t understood exactly what the microglia are doing and whether they are significant in the initial Alzheimer’s process,” says Kim Green, an associate professor of neurobiology & behavior in the School of Biological Sciences at the University of California, Irvine. “We decided to examine this issue by looking at what would happen in their absence.”
“You don’t have Alzheimer’s without plaques, and we now know microglia are a necessary component in the development of Alzheimer’s.”
The researchers used a drug that blocks microglia signaling that is necessary for their survival. Green and his lab have previously shown that blocking this signaling effectively eliminates these immune cells from the brain.
“What was striking about these studies is we found that in areas without microglia, plaques didn’t form,” Green says. “However, in places where microglia survived, plaques did develop. You don’t have Alzheimer’s without plaques, and we now know microglia are a necessary component in the development of Alzheimer’s.”
The scientists also discovered that when plaques are present, the immune cells perceive them as harmful and attack them. However, the attack also switches off genes in neurons needed for normal brain functioning.
“This finding underlines the crucial role of these brain immune cells in the development and progression of Alzheimer’s,” says Green.
The researchers say their discovery holds promise for creating future drugs that prevent the disease.
“We are not proposing to remove all microglia from the brain,” Green says, noting the importance of microglia in regulating other brain functions. “What could be possible is devising therapeutics that affect microglia in targeted ways.”
He also believes the project’s research approach offers an avenue for better understanding other brain disorders.
“These immune cells are involved in every neurological disease and even in brain injury,” Green says. “Removing microglia could enable researchers working in those areas to determine the cells’ role and whether targeting microglia could be a potential treatment.”
The study appears in the journal Nature Communications. The National Institutes for Health provided support for the research, which took place in collaboration with Plexxikon Inc.
Source: UC Irvine