Kids with public insurance are slightly more likely to receive medical care that they don’t need than those with private insurance, a new study finds.
One in nine publicly insured and one in 11 privately insured children received low-value care in 2014, according to the findings in Pediatrics.
Researchers evaluated data for 8.6 million children in 12 states to see whether having public or private insurance is associated with receiving low-value medical services.
“…children are highly likely to receive wasteful care regardless of what type of insurance they have.”
“In a prior study, we showed that privately insured children frequently received low-value services that do not improve their health, but we didn’t know if publicly insured children were more or less likely to receive wasteful care,” says lead author Kao-Ping Chua, a pediatrician and researcher at Michigan Medicine’s CS Mott Children’s Hospital and the Susan B. Meister Child Health Evaluation and Research Center.
“While we found that publicly insured children were a little more likely to receive low-value services, the difference was not large. The more important finding is that children are highly likely to receive wasteful care regardless of what type of insurance they have. This means that efforts to reduce waste should be global in nature and target the care of all children.”
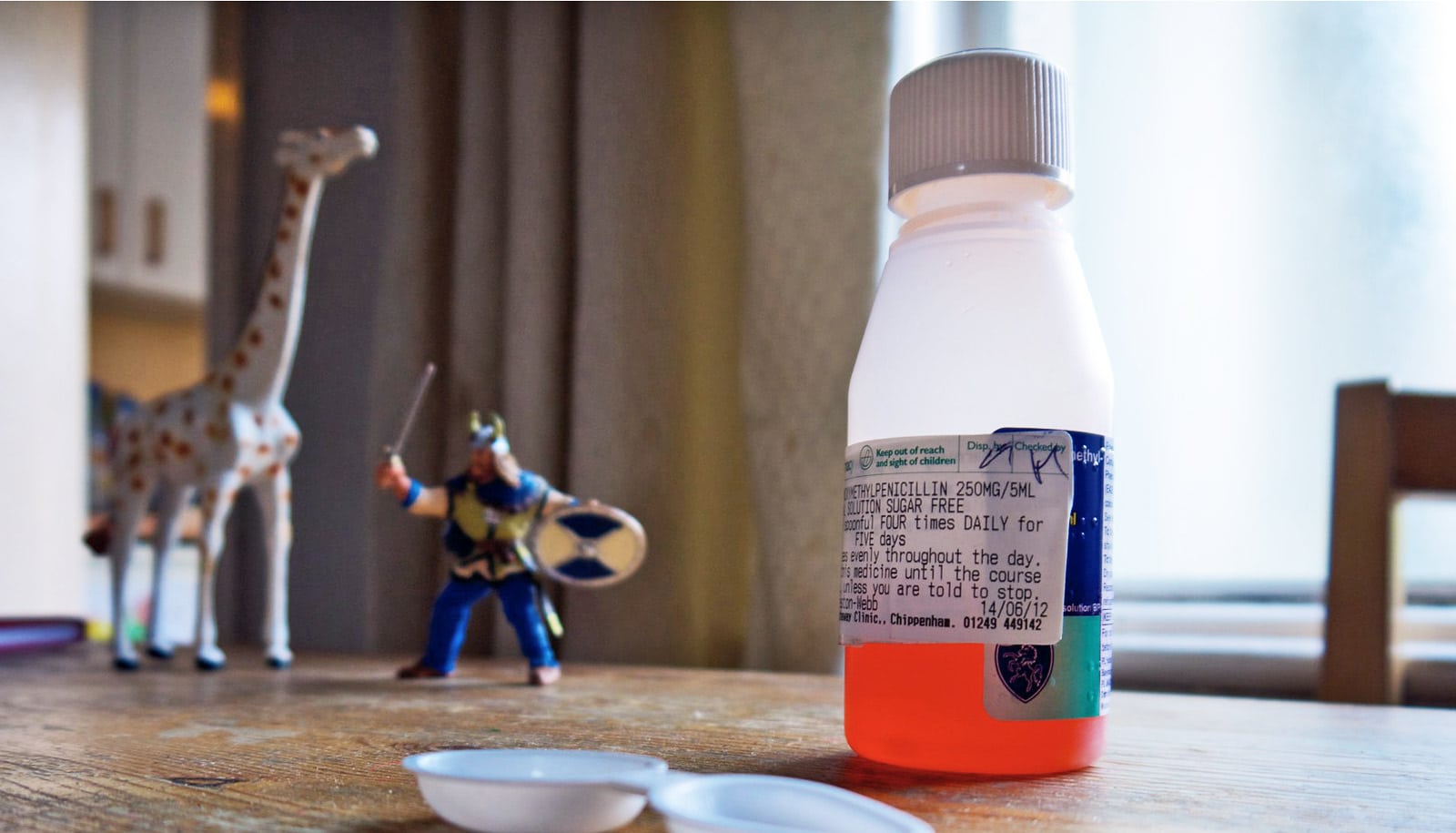
Researchers estimated the prevalence of 20 low-value diagnostic tests, imaging tests, and prescription drugs, such as unnecessary vitamin D screening, imaging for acute sinus infections, and antibiotic prescriptions for colds.
Among publicly and privately insured children in the sample, respectively, 11% and 9% received unnecessary services at least once in 2014 while about 4% and 3% received low-value services at least twice.
About one in 33 publicly and privately insured kids received a low-value diagnostic test at least once in 2014. About one in 12 publicly insured and one in 20 privately insured children received a low-value prescription drug at least once.
“Our study shows that insurance type doesn’t strongly predict whether a child is likely to receive wasteful care,” says Chua, who’s also a researcher at the University of Michigan Institute for Healthcare Policy and Innovation.
Chua points to several factors that may explain why some children still receive low-value services despite evidence that they don’t work. High on the list is the difficulty in changing the interventionist culture of medicine.
“Parents understandably want to relieve their children’s suffering and to rule out serious problems,” Chua says. “Both parents and doctors sometimes have a tendency to believe that prescribing a drug or ordering a test is better than doing nothing, even though the right answer is often to do less.
“The expectation that something be done can be particularly high when parents miss work and children miss school to go to the doctor, or when children previously received an unnecessary intervention for the same condition, like an antibiotic for a cold.”
Some interventions also stem from an overabundance of caution.
“Doctors have a strong fear of missing something,” Chua says. “Some doctors would rather over-treat and risk the side effects of the intervention than under-treat and risk missing a catastrophic problem.”
Unnecessary care has consequences, Chua says. Overuse of antibiotics, for example, can increase antibiotic resistance and the risk of allergic reactions. MRIs sometimes expose children to the risks of sedation while CT scans expose them to radiation, which can increase the lifetime risk of cancer.
All low-value services also come with wasteful healthcare spending, Chua says.
“These interventions waste healthcare dollars that could be devoted to other valuable causes, and also force many families to pay out-of-pocket for unnecessary care,” Chua says. “Reducing wasteful care will improve child health and decrease the financial burden of health care spending on society and families.”
Source: University of Michigan