New biotechnology could speed up the development of medicines to treat pulmonary fibrosis, one of the most common and serious forms of lung disease, research shows.
Developing new medicines isn’t easy, researchers say, because it’s difficult to simulate how the disease damages and scars lung tissue over time. Scientists have to use a hodgepodge of time-consuming and costly techniques to assess the effectiveness of potential treatments.
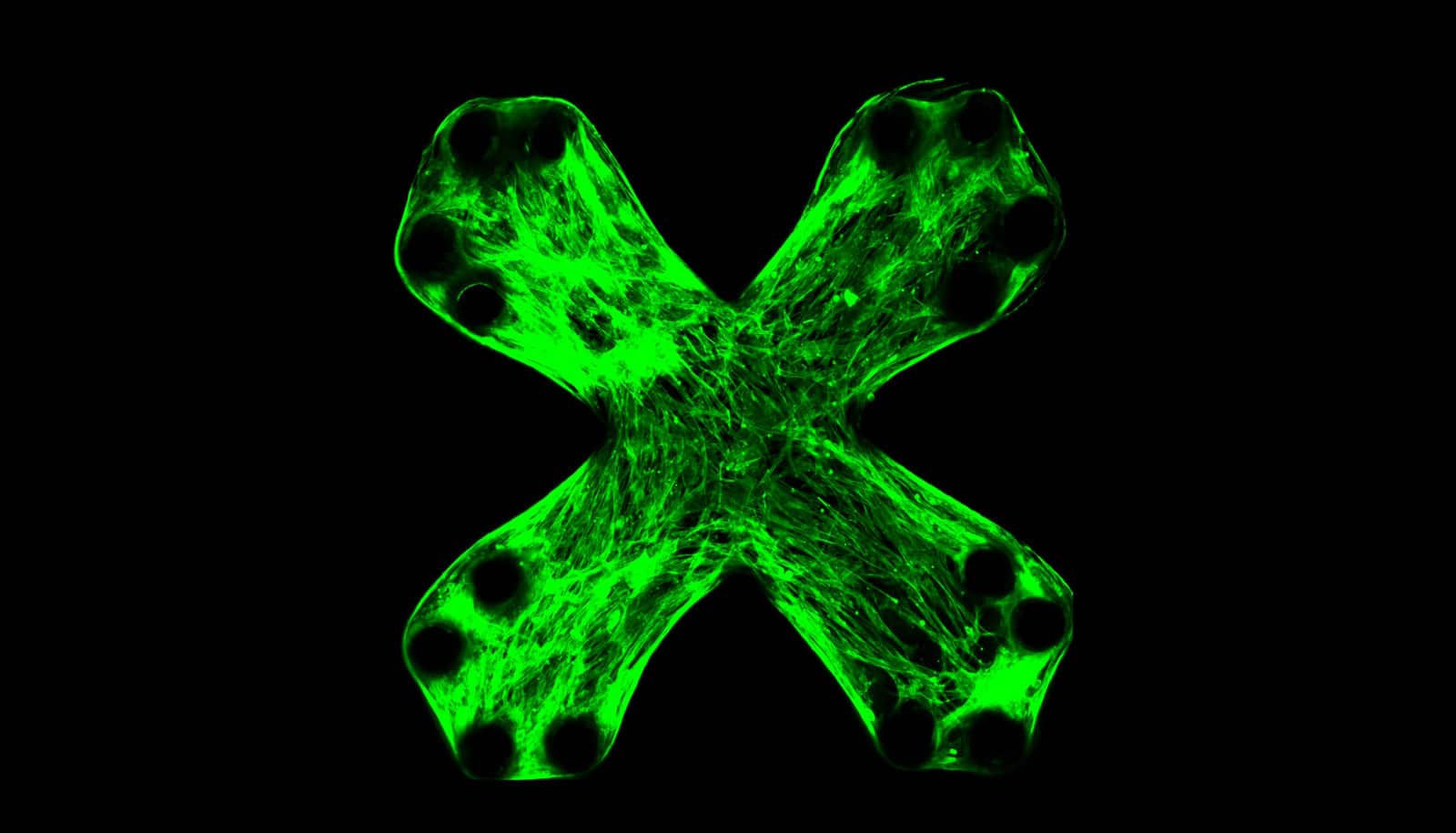
As reported in Nature Communications, the new method relies on the same technology used to print electronic chips—photolithography. Only instead of semiconducting materials, researchers placed arrays of thin, pliable lab-grown lung tissues on the chip.
“Obviously it’s not an entire lung, but the technology can mimic the damaging effects of lung fibrosis,” says lead author Ruogang Zhao, assistant professor in the biomedical engineering department at the University at Buffalo. “Ultimately, it could change how we test new drugs, making the process quicker and less expensive.”
With limited tools for fibrosis study, scientists have struggled to develop medicine to treat the disease. To date, the FDA has approved only two drugs—pirfenidone and nintedanib—that help slow its progress.
However, both drugs treat only one type of lung fibrosis: idiopathic pulmonary fibrosis. There are more than 200 types of lung fibrosis, according to the American Lung Association, and fibrosis also can affect other vital organs, such as the heart, liver, and kidney.
Furthermore, the existing tools don’t simulate the progression of lung fibrosis over time—a drawback that has made the development of medicine challenging and relatively expensive. Using microlithography, researchers printed tiny, flexible pillars made of a silicon-based organic polymer. They then placed the tissue, which acts like alveoli (the tiny air sacs in the lungs that allow us to consume oxygen), on top of the pillars.
These cells turn lung transplants deadly
Researchers induced fibrosis by introducing a protein that causes healthy lung cells to become diseased, leading to the contraction and stiffening of the engineered lung tissue. This mimics the scarring of the lung alveolar tissue in people who suffer from the disease.
The tissue contraction causes the flexible pillars to bend, allowing researchers to calculate the tissue contraction force based on simple mechanical principles.
Big data tool predicts best lung cancer treatment
The system’s effectiveness was tested with pirfenidone and nintedanib. While each drug works differently, the system showed positive results for both, suggesting the lung-on-a-chip technology could be used to test a variety of potential treatments for lung fibrosis.
Researchers from the University of Toronto also contributed to the study. The National Institutes of Health and UB’s School of Engineering and Applied Sciences; Jacobs School of Medicine and Biomedical Sciences; and Clinical and Translational Science Institute funded the work.
Source: University at Buffalo