Researchers have discovered that chronic symptoms in long COVID are, to some extent, due to a part of our immune system called the complement system.
Long COVID patients have chronic symptoms such as fatigue or shortness of breath.
The new study identified a pattern in the blood proteins that will improve the diagnosis and perhaps also the targeted treatment of long COVID.
Most people infected with the SARS-CoV-2 virus recover after the acute illness. However, a significant proportion of infected individuals develop long-lasting symptoms with a wide range of manifestations. The causes and disease mechanisms of long COVID are still unknown, and there are no diagnostic tests or targeted treatments.
A team of researchers led by Onur Boyman, professor of immunology at the University of Zurich (UZH) and director of the immunology department at the University Hospital Zurich (USZ), has shown in the new study that the complement system plays an important role in long COVID. It is part of the innate immune system and normally helps to fight infections and eliminate damaged and infected body cells.
“In patients with long COVID, the complement system no longer returns to its basal state, but remains activated and, thus, also damages healthy body cells,” says Boyman.
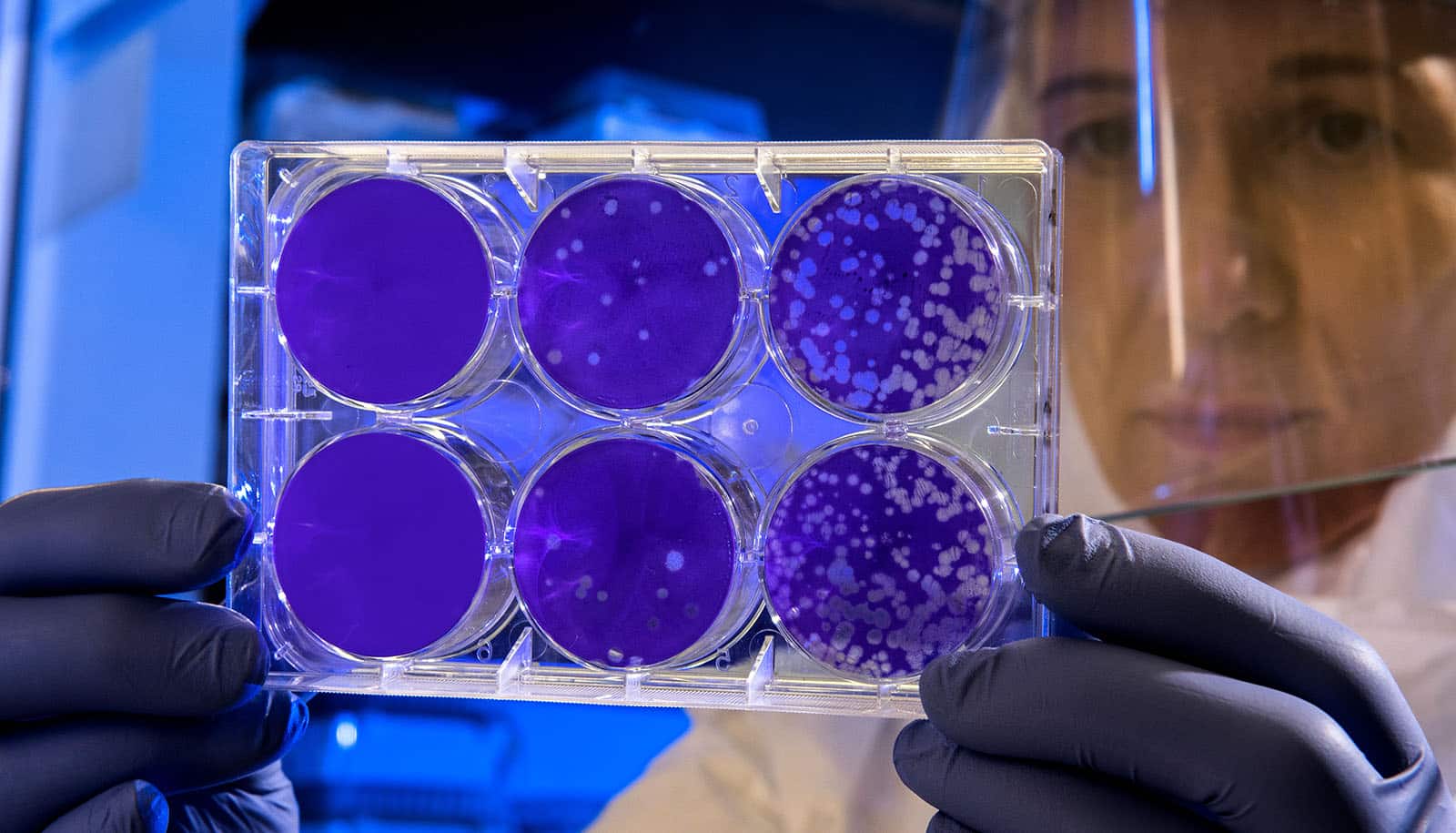
The researchers followed 113 COVID-19 patients for up to one year after their acute SARS-CoV-2 infection and compared them with 39 healthy controls. After six months, 40 patients had active long COVID disease. More than 6,500 proteins in the blood of the study participants were analyzed both during the acute infection and six months later.
“The analyses of which proteins were altered in long COVID confirmed the excessive activity of the complement system. Patients with active long COVID disease also had elevated blood levels indicating damage to various body cells, including red blood cells, platelets, and blood vessels,” explains Carlo Cervia-Hasler, a postdoctoral researcher in Boyman’s team and first author of the study.
The measurable changes in blood proteins in active long COVID indicate an interaction between proteins of the complement system, which are involved in blood clotting and the repair of tissue damage and inflammation. In contrast, the blood levels of long COVID patients who recovered from the disease returned to normal within six months. Active long COVID is therefore characterized by the protein pattern in the blood. The blood markers were discovered using bioinformatics methods in collaboration with Karsten Borgwardt during his time as a professor at ETH Zurich.
“Our work not only lays the foundation for better diagnosis, but also supports clinical research into substances that could be used to regulate the complement system. This opens up new avenues for the development of more targeted therapies for patients with long COVID,” says Boyman.
The research appears in Science.
Source: University of Zurich