Researchers have created a high-resolution picture of the cells at work inside a key hub of metabolism—the liver—and how disease reprograms individual cell types.
In every tissue throughout our bodies, various cell types communicate and coordinate their efforts to perform vital functions and maintain health.
The new research not only reveals a detailed map of cell-to-cell signaling in the liver, but also identifies cellular changes that could potentially drive the progression of nonalcoholic steatohepatitis, or NASH, a severe form of fatty liver disease with no effective therapies.
Until recently, scientists could analyze what was occurring only across a mixture of cells in a specific organ or tissue. But they lacked the technology to decipher the distinct cells within that complex mixture and see how each type involved in overall tissue health and function.
“That was one question we really wanted to address with this study: Can we have a high-definition picture of each cell type in the liver, what signaling molecules are being released by each of these different cell types, and what they are capable of responding to?” says Jiandie Lin, a professor at the Life Sciences Institute at the University of Michigan and senior author of the paper in Molecular Cell. “Now, with the new single-cell RNA sequencing technology, we can do that.”
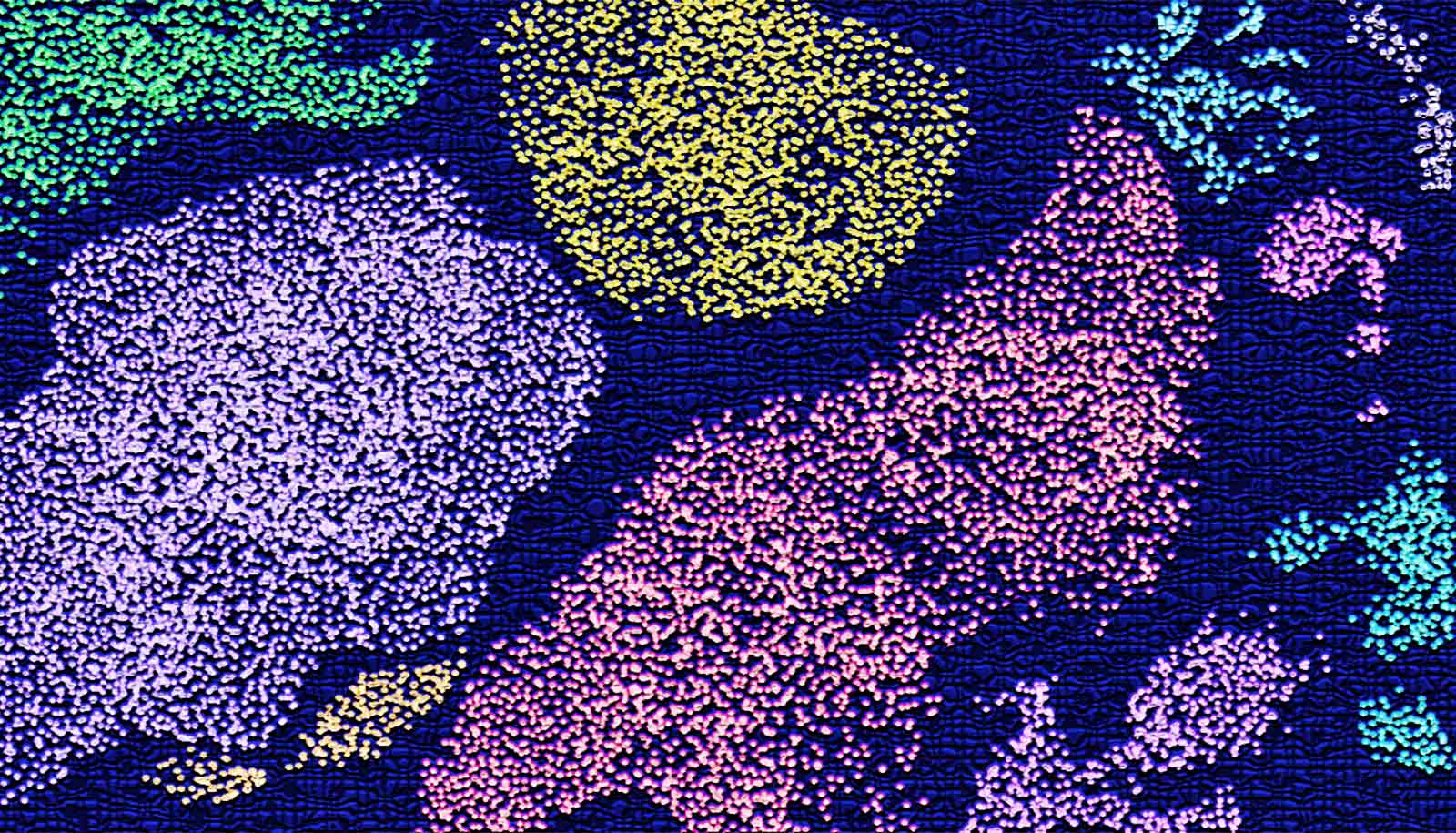
Mapping liver cells
Single-cell sequencing allows researchers to isolate cells from a tissue sample and then determine the precise order of nucleic acids—the molecules that make up DNA and RNA—within each cell. Researchers can use this information to discover new cell types and activities within the tissue.
Lin and his colleagues used the new tool to obtain a gene expression profile for individual liver cells. Comparing data from mouse and human livers, the researchers laid out a blueprint of the types of cells operating in the liver, which signals the cells produce, and which cells receive those signals. The information provides unprecedented details that help create a high-definition map of cell signaling in the liver.
They also compared healthy livers with diseased livers to determine how cellular properties change in NASH livers. Patients with this severe form of fatty liver disease are more likely to experience cirrhosis and liver cancer. Researchers commonly associate NASH with metabolic syndrome; however, the exact triggers that drive disease progression remain poorly understood.
“We wanted to decode what exactly is going on for each cell type during disease,” says Lin, who is also a professor of cell and developmental biology. “Can we uncover new biology, new disease mechanisms, maybe even new therapeutic targets using single-cell analysis?”
Cellular surprise
Using a mouse model of NASH, the researchers found that the abundance of cells within the liver changed with disease, but so did the properties of each cell type. In particular, cells called macrophages were present at substantially higher proportions in diseased livers and were more actively producing a protein called Trem2 (for “triggering receptors expressed on myeloid cells 2”).
Researchers also observed the emergence of Trem2-marked macrophages in the livers from a cohort of human NASH patients. What’s more, the presence of Trem2 was also associated with disease severity—as the liver became more diseased, the cells produced more Trem2; as NASH improved, Trem2 levels decreased.
And the analysis of single cells also revealed new information about star-shaped cells, called hepatic stellate cells, known to contribute to liver fibrosis. In this new study, the researchers discovered that stellate cells are actively secreting various signaling molecules, dubbed “stellakines,” and respond to hormones that typically act on blood vessels in the body.
“The findings on hepatic stellate cells really surprised us,” says lead author Xuelian Xiong. “And they highlight the power of single-cell biology in discovering new modes of cell communication and function.”
Additional authors are from the University of Michigan; the University of California, Los Angeles; Instituto Nacional de Ciencias Medicas y Nutricion; Unidad de Genómica de Poblaciones Aplicada a la Salud; and the University of Texas Southwestern Medical Center.
The National Institutes of Health, Michigan Diabetes Research Center, Welch Foundation, UCLA Clinical and Intramural Award, and the University of Michigan supported the work.
Source: University of Michigan