A new “lab-on-a-chip” can examine thousands of individual live cells over a weeklong period, performing experiments that would take more than 1 million steps in a laboratory.
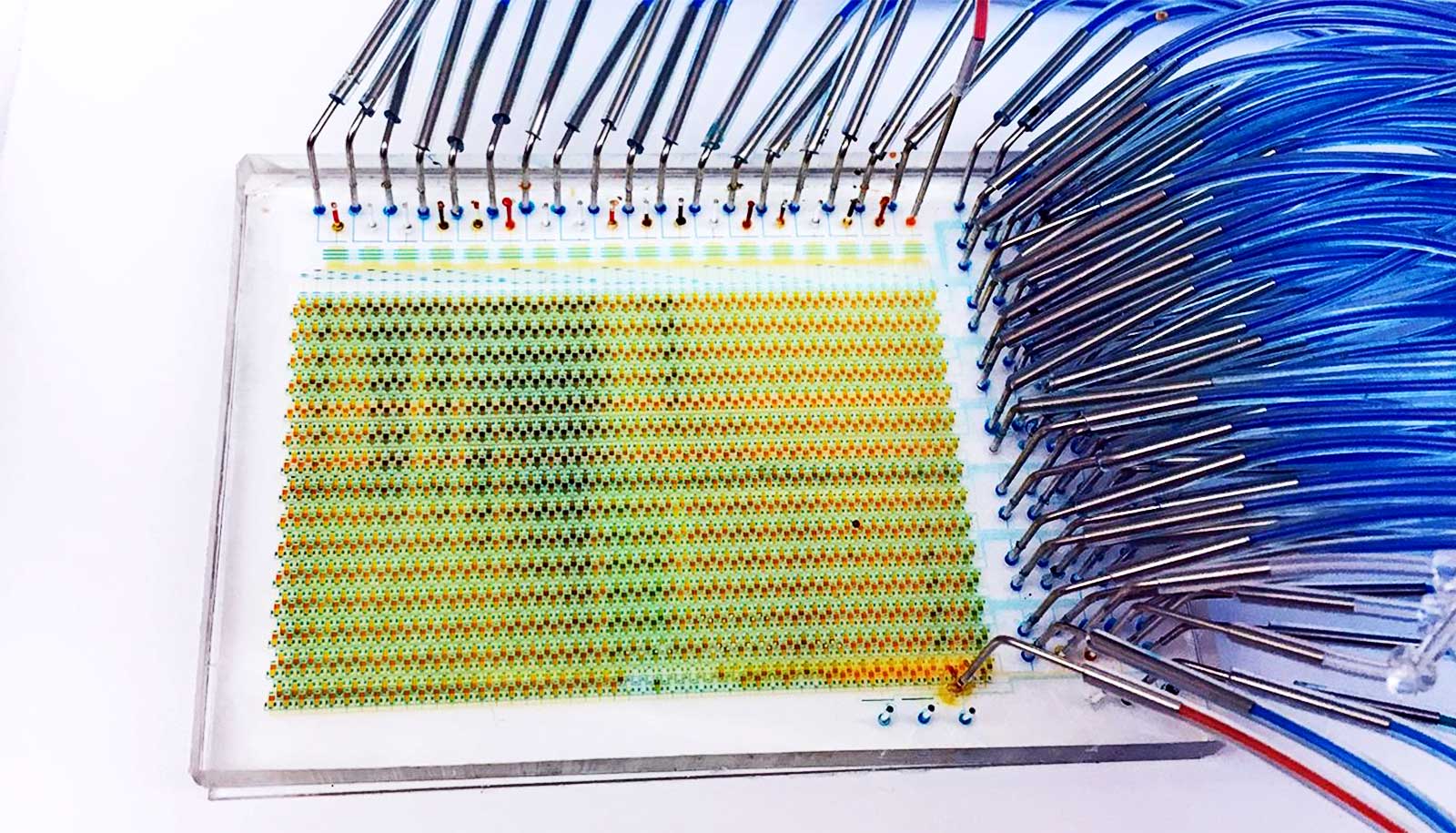
The credit-card-sized, microfluidic device not only saves time and money, but also offers a new glimpse into how single stem cells react to different molecules and environments.
When researchers examined neural stem cells on the device and analyzed the data, they found several new rules that determine the timing and signaling sequences necessary for the cells to differentiate or renew themselves. The finding could have implications in understanding brain development or in treating patients with immunotherapy.
“We wanted to develop a microfluidic device that could sort, image, and culture single cells in an automated, high-throughput way,” says Savas Tay, associate professor at the University of Chicago and lead author of the research, which appears in Science Advances.
“We achieved that, and now we have an understanding of how stem cells make decisions. That’s pretty exciting.”
Multitasking device
Cells in our body constantly respond to different signals and changes in the environment. In stem cells, for example, signals received at different points in time determine how the cell chooses what kind of cell it will develop into. One signal might cause a stem cell to differentiate into another cell, while another signal might cause it to maintain its form.
Researchers currently have no way of studying these signal molecules on individual cells inside the body. Scientists can do such analysis in a lab with expensive, time-consuming experiments, but they ultimately cannot test all possible outcomes.
Microfluidic devices, which have tiny chambers, tunnels, and valves, offer researchers a faster, automated process for studying these reactions in cells. But past devices have offered a limited number of chambers—meaning researchers could only test a certain number of conditions with each cell—and could not keep the cells alive long enough to study them over a long period of time.
Tay and colleagues set out to change that. They designed a microfluidic device that has 1,500 automated chambers—much higher than similar devices, which have less than 100. The device can also conduct several tasks—like cell stimulation, culturing, imaging, and sorting—previously relegated to separate devices. It can also culture cells in different modes—meaning it can examine different types of cells at the same time.
Finally, the device also can keep cells alive for much longer, thanks to a new technique of diffusing media into a cell culture.
Normally, to keep cells alive, researchers need to change the media where they are every few hours. But this change shocks the cells, and after several shocks, the cells can die. The researchers’ new technique diffuses the media into the cell chamber, a gentler process that doesn’t shock the cells.
Millions of data points
In their first experiment with the device, the researchers studied how different signaling molecules affect the outcome of mouse neural stem cells. Such experiments create millions of data points, so Tay collaborated with Andrey Rzhetsky, professor in medicine and genetics, to conduct machine-learning analyses on the large dataset.
They found that certain combinations of signals synergize and cause the cells to differentiate, while other molecules shut down those processes. The timing of these signals is also crucial. If a molecule delivery happens at the right time, it can change the course of stem cells, from differentiation to self-renewal.
“There are certain orders of signals that are highly optimal, and the exact timing of signals matters,” Tay says. “There hasn’t been a way to dynamically monitor these cells before, so finding and understanding these principles is exciting.”
Next, the researchers hope to use the device to study organoids, tissue cultures derived from stem cells that organize themselves like tiny organs.
Ultimately, scientists could use a device like this in fields like immunotherapy, where they can stimulate a patient’s own immune system to help fight disease. Doctors could remove a patient’s stem cells, place them into the device and give them the right combination of molecules to develop into a certain lineage, then place them back in the body.
“We want to be able to use this device for all kinds of problems in cell biology,” Tay says.
Additional researchers are from the University of Chicago and the University of Basel. Swiss Initiative in Systems Biology funded the work.
Source: Emily Ayshford for University of Chicago