New research identifies the likely culprit that turns classical Klebsiella pneumoniae into a devastating, drug-resistant killer.
More than a decade ago, physicians around the world began reporting cases due to a new hypervirulent strain of Klebsiella pneumoniae, which could infect and severely sicken otherwise healthy people.
Thomas A. Russo at the University at Buffalo and the VA Western New York Healthcare System (VAWNYHS) was one of them. In 2011, he treated his first case in Buffalo, a young person with no other comorbidities who was hospitalized for months with this hypervirulent bacterium.
The patient fully recovered, but Russo became curious about this hypervirulent bacterium—and alarmed, given the fact that it was able to infect otherwise healthy individuals from the community and, over time, could become drug-resistant.
That alarm was well-founded. The hypervirulent bacteria has spread throughout the world. It can cause tissue-invasive infections that are organ- and life-threatening in healthy people. Some strains have acquired resistance to antimicrobial agents; these strains have been dubbed “true and dreaded superbugs.”
Earlier this year, the European Centre for Disease Control and Prevention of the European Union reported a significant increase in the number of cases of hypervirulent Klebsiella pneumoniae and that these cases were resistant to the class of antibiotics called carbapenems, which are often a “last resort” treatment for bacterial infections.
Now, with numerous publications on the bacterium, Russo has identified the genetic elements responsible for turning classical Klebsiella pneumoniae, which generally infects only sick and/or immunocompromised people in the health care setting, into hypervirulent Klebsiella pneumoniae, which can also infect otherwise healthy people in the community.
Published in eBioMedicine, the research is the first to determine the relative contribution of several key genetic elements to the hypervirulence of this bacterium.
“Our goal with this study was to decipher how several genetic factors contribute to this hypervirulence in order to guide the development of preventive therapies, treatments, and control strategies for hypervirulent Klebsiella pneumoniae,” says Russo, senior author and a professor and chief of the Division of Infectious Diseases in the Jacobs School of Medicine and Biomedical Sciences.
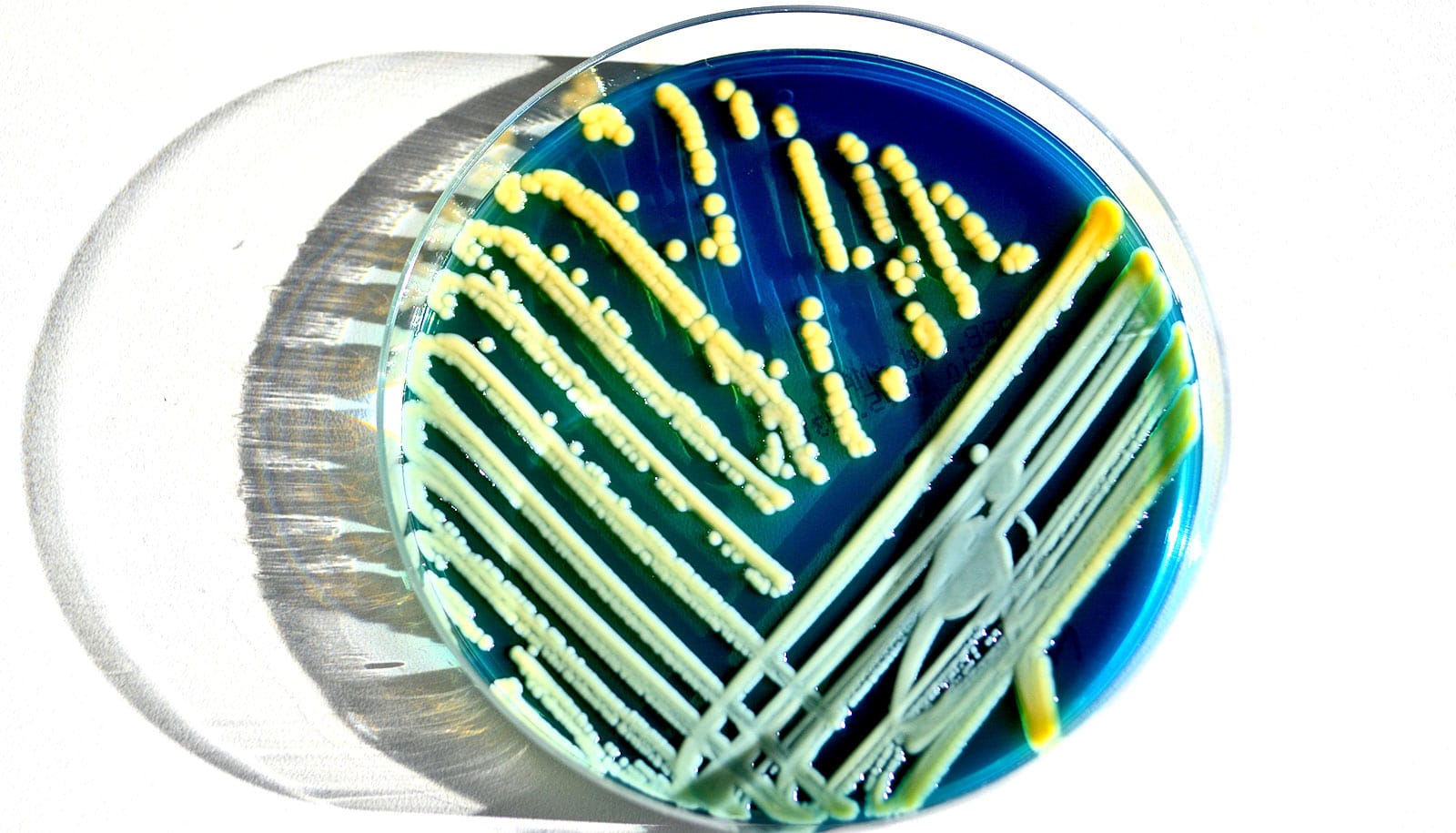
To accomplish this, the researchers conducted a systematic investigation of four representative clinical strains of hypervirulent Klebsiella pneumoniae. They did this by constructing and testing mutants in which pVir, the large plasmid possessed by hypervirulent Klebsiella pneumoniae strains, and other virulence factors alone or in combination were removed.
Russo explains that plasmids are genetic elements separate from the chromosome. They contain multiple genes, some of which may enhance virulence and/or confer resistance to selected antimicrobial agents.
“While the plasmid was known to contribute to hypervirulence in Klebsiella pneumoniae, its relative role and the relative role of selected virulence factors encoded on the plasmid or the chromosome were not well-defined,” says Russo.
The findings strongly supported that pVir is the primary genetic determinant that transforms the baseline virulence potential of classical K. pneumoniae strains to that observed for hypervirulent Klebsiella pneumoniae strains. Data also supports the existence of additional virulence factors encoded by pVir that have yet to be identified.
“The genetic factors defined as being the most quantitively important could be potential therapeutic targets for the development of counter measures,” says Russo.
Previous work published by his group in mBio found that a strain is likely to be hypervirulent if it contains five specific genes located on the plasmid. That work may be critical to developing a diagnostic test for hypervirulent Klebsiella pneumoniae. Presently, clinical microbiology laboratories are unable to differentiate classical from hypervirulent Klebsiella pneumoniae.
Additional coauthors are from the University at Buffalo; the Roswell Park Comprehensive Cancer Center; and the Multidrug-Resistant Organism Repository and Surveillance Network, Walter Reed Army Institute of Research.
Support for this work came from the National Institutes of Health and the Department of Veterans Affairs, and was partially funded by the US Defense Health Program.
Source: University at Buffalo