New research establishes a link between irritable bowel syndrome and mental health challenges, such as anxiety, depression, and suicidal ideation.
The research highlights the need for health professionals to evaluate and treat associated psychiatric comorbidities in irritable bowel syndrome (IBS) patients to improve their overall health and quality of life.
IBS is a chronic disorder of the stomach and intestines affecting up to 15% of the population. It causes cramping, abdominal pain, bloating, gas, and diarrhea.
For the new study, researchers looked at more than 1.2 million IBS patient hospitalizations from 4,000 US hospitals over a three-year period and found that more than 38% had anxiety and more than 27% had depression. Both figures were double the rate of anxiety and depression found in those without IBS.
The prevalence of psychiatric problems including anxiety, depression, bipolar disorder, suicidal attempt/ideation, and eating disorders was significantly higher in the IBS patient population when compared to the general adult population.
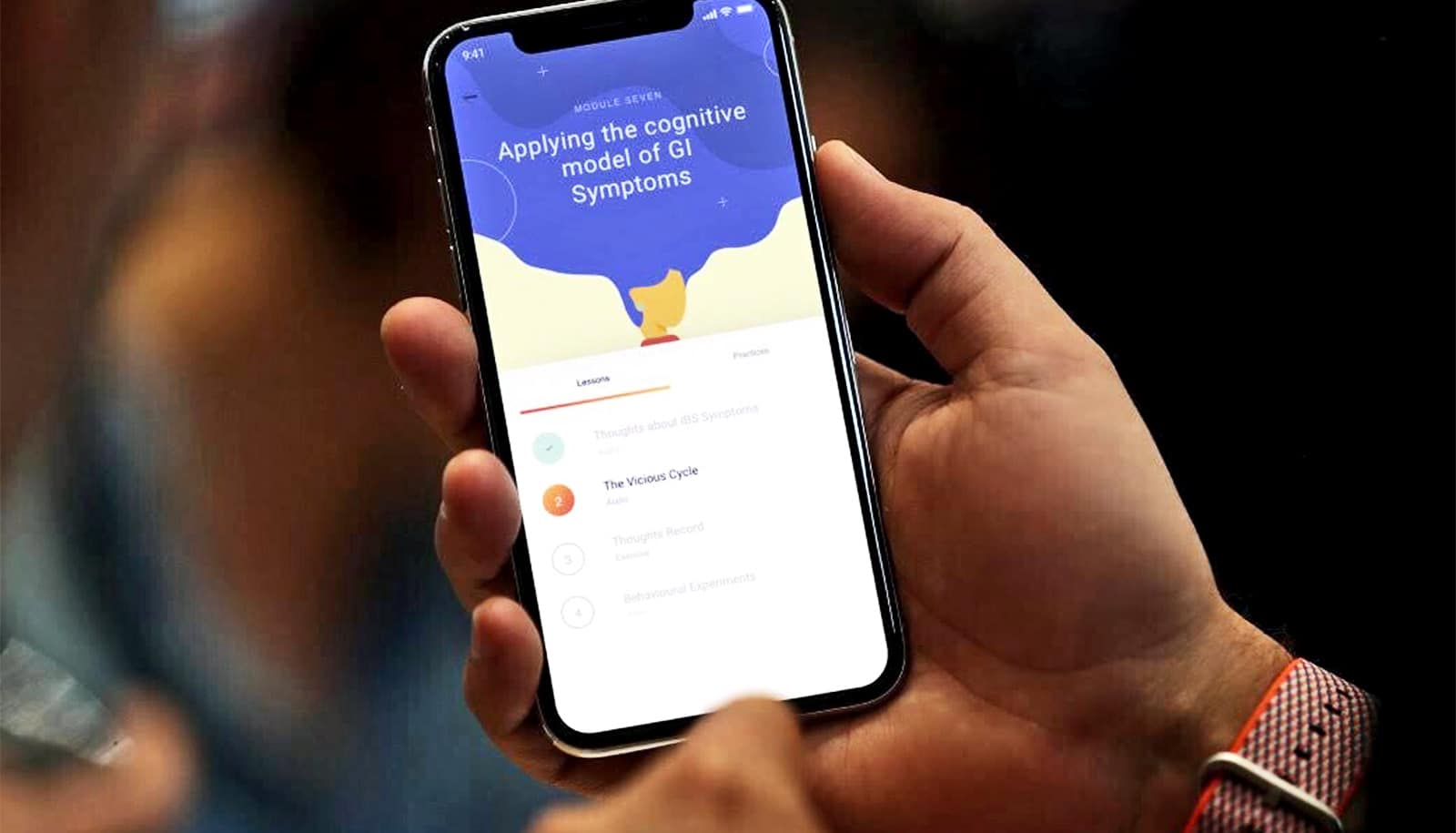
“One possible explanation is the so-called brain-gut axis,” says lead researcher Zahid Ijaz Tarar, assistant professor of clinical medicine at the University of Missouri. “We’ve long suspected that dysfunction of the brain-gut axis is bidirectional, such that IBS symptoms influence anxiety and depression, and on the other hand, psychiatric factors cause IBS symptoms. Medical professionals need to treat both ends of the axis.”
Untreated psychiatric disorders among IBS patients also puts additional strain on health care systems through increased frequency of hospital admissions and longer stays. Chronic diseases like IBS are also known to be associated with stress, work impairment, and associated economic burdens on patients and their families.
“I frequently tell my patients who have IBS, that if they have any type of psychologic stress, it will get expressed in some form or the other,” says senior author Yezaz Ghouri, assistant professor of clinical medicine and gastroenterology.
“The mesentery membrane that holds the intestines together has one of the largest collections of nerve cells in the body. When those nerves start firing impulses, that can lead to the state of nervousness in and around the GI tract, resulting in IBS symptoms. The resulting decline in patient quality of life can lead to poor lifestyle choices, such as smoking. Early evaluation and treatment of both IBS and associated psychiatric conditions is essential.”
The study appears in the Irish Journal of Medical Science. The authors declare that they have no conflicts of interest related to the study.
Source: University of Missouri