Treating children with intravenous antibiotics at home is safe and effective, and compared with hospitals, significantly more cost-effective for the health system and families, according to new research.
Laila Ibrahim, a researcher at the Murdoch Children’s Research Institute and PhD candidate in the pediatrics department at the University of Melbourne Medical School and Penelope Bryant, an assistant professor in the pediatrics department, explain their work here:
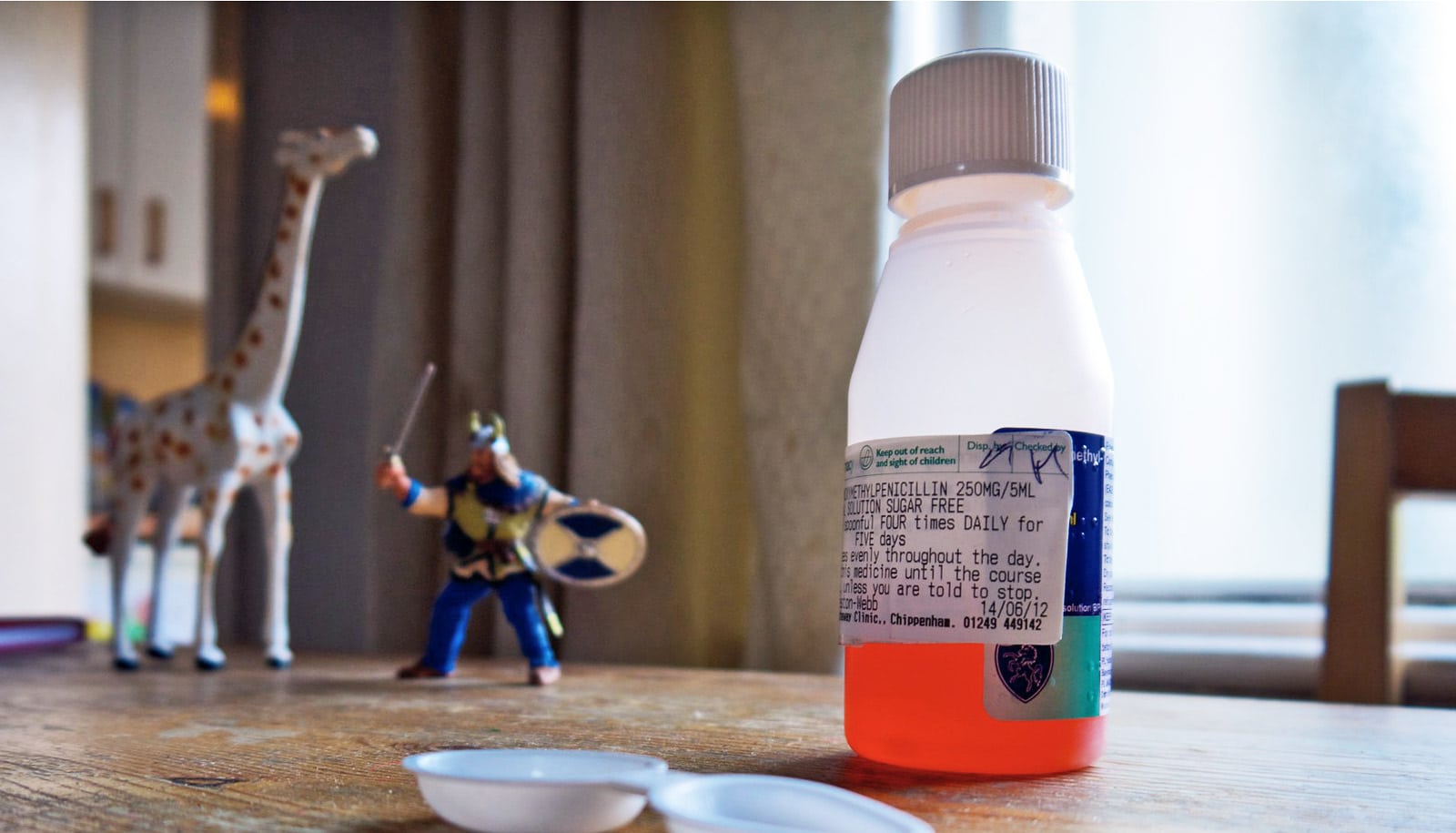
No sick child wants to be in hospital; they want to be home with their families and their pets, in their own room and in their own bed.
We know this instinctively (we were all children once), but research also tells us that being in the hospital weighs on a child’s mental and emotional health. Hospitals also disrupt the whole family unit and puts children at risk of picking up unrelated infections from the hospital environment.
But when it comes to sick children who come into hospital emergency departments, the default treatment pathway is often to admit them. This needn’t be the case.
One common reason why children are admitted to the hospital is to be treated with intravenous antibiotics, where the medication is delivered directly into the blood stream through a drip.
Now, for the first time, our research has shown that administering intravenous antibiotics at home is just as effective and safe as in a hospital, if not more so. And, it comes at almost half the cost.
Fighting infection with IV antibiotics
Intravenous antibiotics are often used to fight rapidly spreading infections like, for example, the bacterial skin infection cellulitis.
Antibiotics delivered directly into the bloodstream can start acting against infections much quicker than oral antibiotics which need to be swallowed, absorbed by the gut, and finally metabolized in the liver before they become effective.
For children in particular, clinicians may choose intravenous antibiotics to tackle fast spreading infections or if oral antibiotics cause nausea and vomiting.
Because it spreads rapidly, but is usually not dangerous, cellulitis was an ideal infection for us to test whether we can treat children with intravenous antibiotics at home just as well as in the hospital.
Hospitals vs. home
Our study, published in Lancet Infectious Diseases, included 188 children (aged from six months old up to 18 years old) with moderate-to-severe cellulitis.
Half were randomly chosen to be treated with intravenous antibiotics in the hospital, while the other half were treated at home by having a doctor and nurse attend to administer the intravenous antibiotics.
Among the children treated at home, only 2% experienced some sort of initial treatment failure, much less than among the children in the hospital where 7% experienced treatment failure.
Treatment failure was defined as when the initial antibiotics had to be switched for another either because it wasn’t working, or because it resulted in an adverse responses like redness, swelling, pain, or fever.
The lower treatment failure at home may partly reflect the intensity of medical care in hospital settings where doctors may feel under pressure to switch to a different medication too early.
Importantly, adverse events like diarrhea and vomiting occurred less at home than in the hospital, potentially because in some cases the diarrhea and vomiting may have been due to a separate infection picked up in the hospital.
Less costly
We also surveyed parents and children on their satisfaction with treatment and its impact on their quality of life. Families expressed high satisfaction when treated at home, and the children themselves reported experiencing significantly higher quality of life compared to children treated in the hospital.
Given the convincing better outcomes for home treatment, it would be reasonable to think that the cost would be higher for nurses and doctors to administer care in the home compared to in the hospital. Wrong.
The results of our cost-effectiveness analysis showed that the institutional cost per child treated in the hospital was $A3,775 ($2544.65 USD) over the two days of treatment, almost double the cost of treating the home-based group at $A1,965 ($1324.57 USD) per child.
The average cost incurred by each family was $A593 ($399.73 USD) for the hospital group and just $A182 ($122.68 USD) for the home group. This cost included time off work and expenses like transport, food, or extra childcare costs, all of which are costs not covered by Medicare—Australia’s government healthcare funder.
Families then, are facing a cost burden that is three times more when their child is treated in the hospital compared to at home, a factor often overlooked by doctors.
Our study showed that parents or guardians had to take two days off work if their child was treated at hospital, compared to less than a day if treated at home.
The potential for savings both for the health system and for individuals is enormous.
Hospitals could save a collective $A4.3 million (about $2.9 million USD) a year nationally and families a collective $A990,150 ($667,440.31 USD), just in the treatment of cellulitis. This is based on a conservative estimate that 2,415 children a year attend emergency departments with cellulitis, who would be treatable at home.
Home care
As we attempt to move towards sustainable healthcare by allocating resources effectively, translating care from hospitals to people’s homes will be a key way to keep health costs affordable for government and families.
Previous research on moving healthcare into homes, has largely been focused on adults and children who have chronic health conditions.
What makes our study cutting-edge is that the children in our study had an acute condition and completely avoided hospital admission by going home directly from the emergency department.
Currently, worldwide the standard of care for children who need intravenous antibiotics is to admit them to the hospital. But our findings should change the way clinicians consider care in Australia and internationally. These results provide the first robust evidence to support the expansion of hospital-level care at home.
No sick child wants to be in hospital. Perhaps they don’t have to.
Source: University of Melbourne