Bioscientists are moving closer to 3D-printed tissues to help heal bone and cartilage damaged in sports injuries to knees, ankles, and elbows.
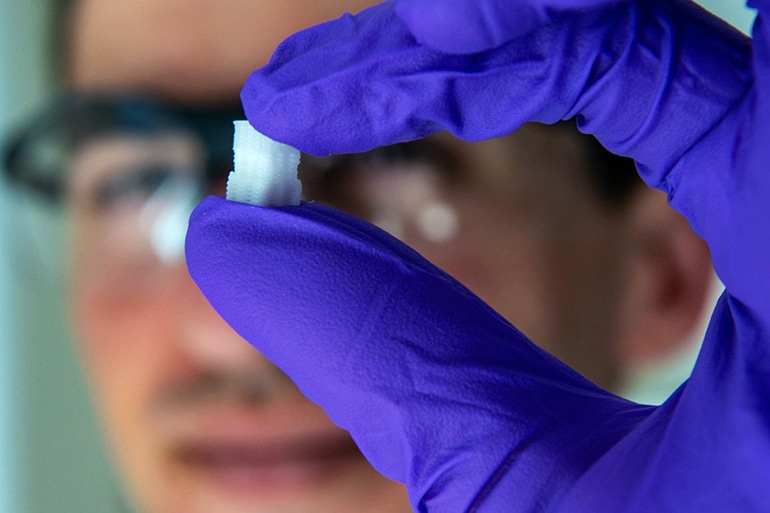
Scientists engineered scaffolds that replicate the physical characteristics of osteochondral tissue—basically, hard bone beneath a compressible layer of cartilage that appears as the smooth surface on the ends of long bones.
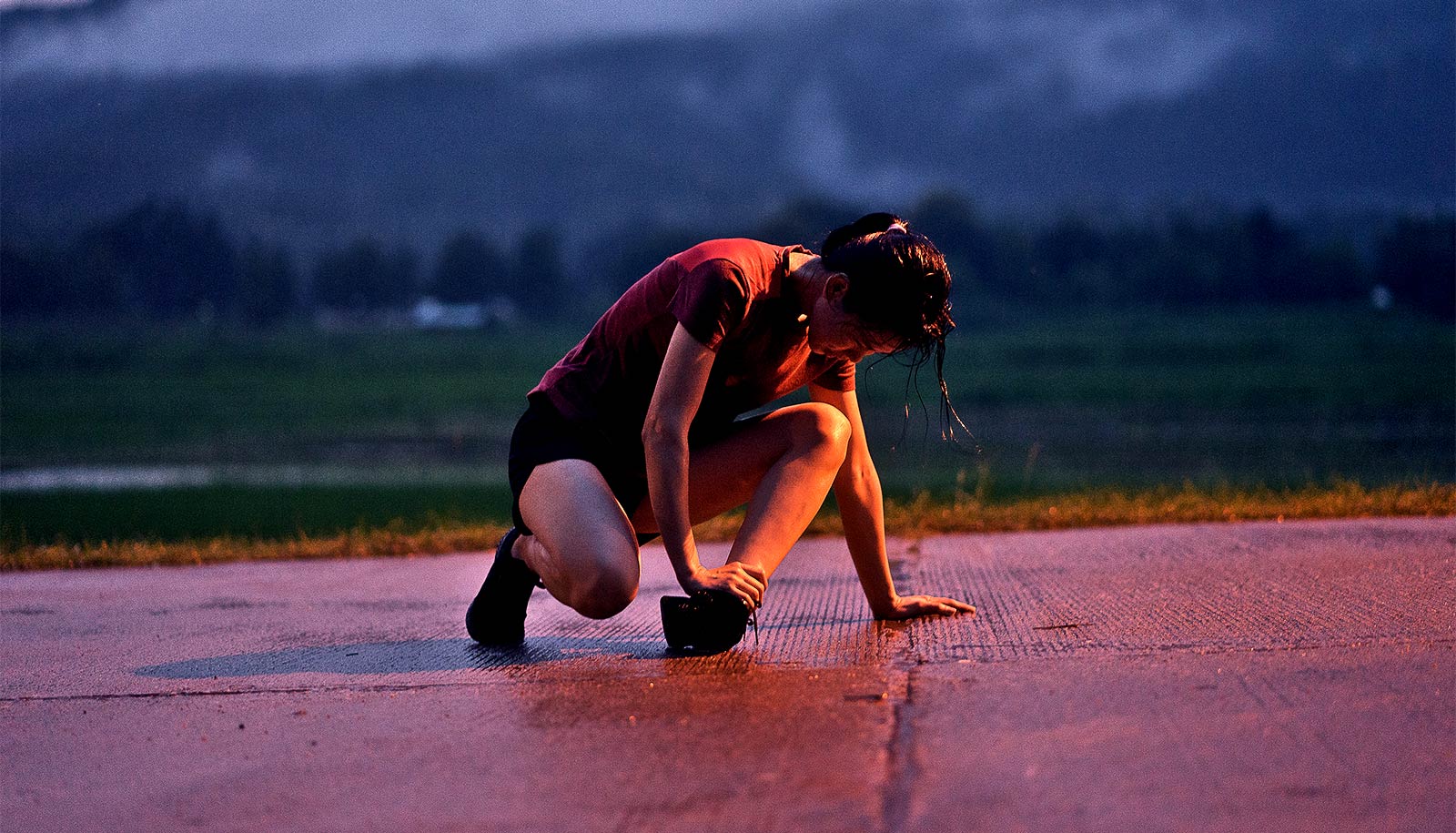
Injuries to these bones, from small cracks to pieces that break off, are painful and often stop an athlete’s career in its tracks. Osteochondral injuries can also lead to disabling arthritis.
The gradient nature of cartilage-into-bone and its porosity have made it difficult to reproduce in the lab, but Antonios Mikos, a bioengineer at Rice University and graduate student Sean Bittner used 3D printing to fabricate what they believe will eventually offer a suitable material for implantation.
“Athletes are disproportionately affected by these injuries, but they can affect everybody,” says Bittner, who is also a a National Science Foundation fellow and lead author of the paper, which appears in Acta BioMaterialia. “I think this will be a powerful tool to help people with common sports injuries.”
The key is mimicking tissue that turns gradually from cartilage (chondral tissue) at the surface to bone (osteo) underneath. The researchers printed a scaffold with custom mixtures of a polymer for the former and a ceramic for the latter with imbedded pores that would allow the patient’s own cells and blood vessels to infiltrate the implant, eventually allowing it to become part of the natural bone and cartilage.
“For the most part, the composition will be the same from patient to patient,” Bittner says. “There’s porosity included so vasculature can grow in from the native bone. We don’t have to fabricate the blood vessels ourselves.”
The future of the project will involve figuring out how to print an osteochondral implant that perfectly fits the patient and allows the porous implant to grow into and knit with the bone and cartilage.
Additional coauthors are from Rice, the University of Maryland, and Wake Forest School of Medicine. The National Institutes of Health and the RegenMed Development Organization supported the research.
Source: Rice University