A new technique could lead to an oral hepatitis B vaccine.
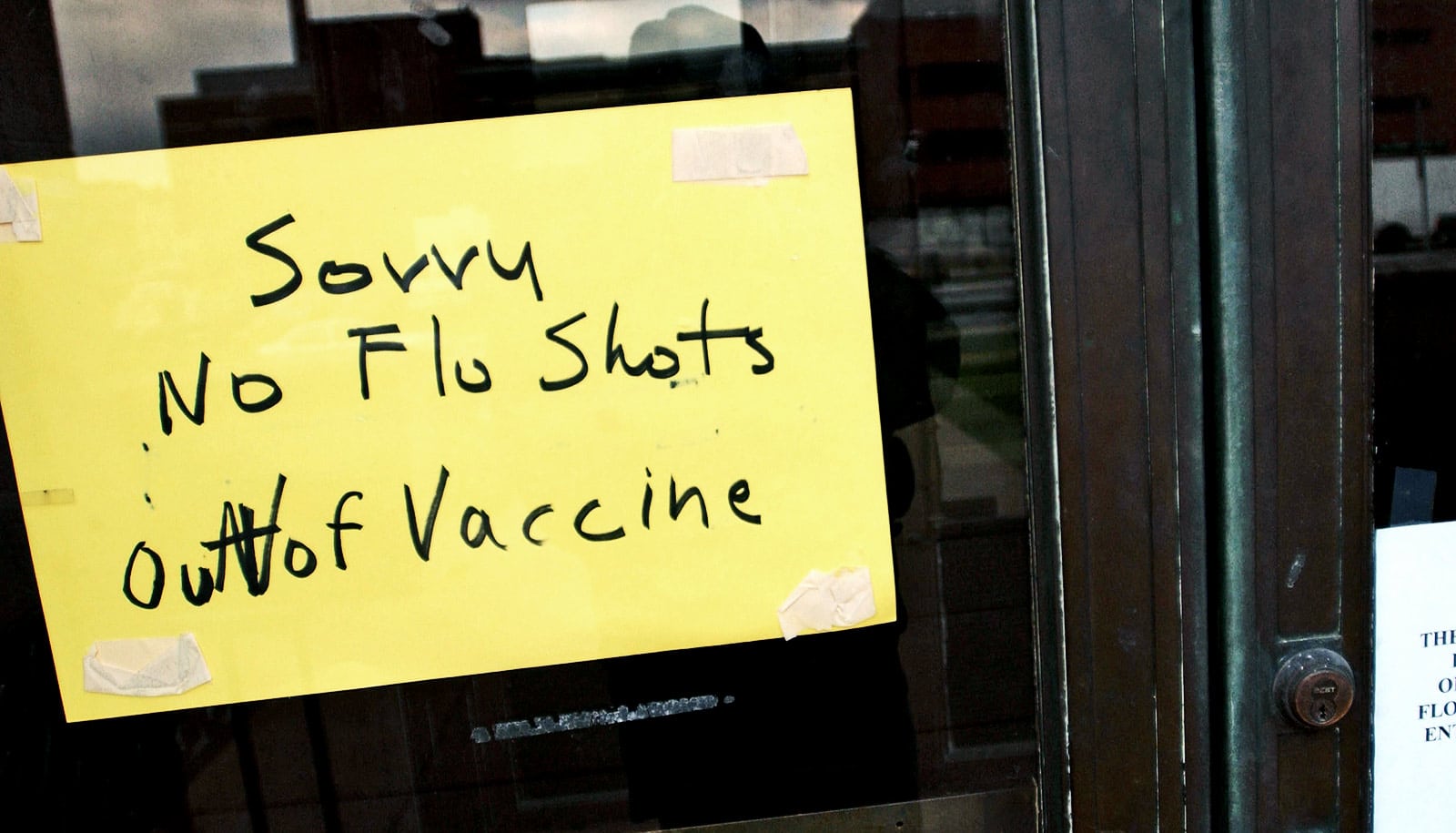
Hepatitis B infects millions of people every year. Hundreds of thousands die. And small children are particularly at risk. Due to high cost and the stable environmental conditions required for vaccine storage, many people in developing countries don’t receive vaccines against this dangerous virus.
As such, researchers have been working to produce a drop or powdered form of oral vaccine. Oral vaccinations are cheaper and easier to administer than injections. However, developing a sufficiently effective oral hepatitis B vaccine has eluded researchers until now.
“We have used a technology commonly used in solid state physics to explore how the vaccine behaves within a particular type of encapsulation. This has yielded crucial information that would not otherwise have been achievable,” says coauthor Heloisa Bordallo, an associate professor at the Niels Bohr Institute at the University of Copenhagen, and one of the two main authors of an article in Scientific Reports about the work.
Inside silica
A major challenge of making an oral vaccine is to encapsulate it in a material that can endure the harsh conditions of our digestive system, to protect the vaccine from being destroyed before it reaches its intended destination in the body.
Collaborators in Brazil have long known that the silica-material SBA-15 is well-suited to encapsulate a hepatitis B vaccine. However, they did not know exactly how the material protected the vaccine, nor were they certain about why their vaccine was not always completely effective.
Using a special technique that combines X-ray and neutron imaging, the team of Danish physicists produced 3D images of the inside of the SBA-15 silica. It marked a crucial step in the use of this technique to develop pharmaceuticals.
The imagery allows researchers to see how the vaccine behaves inside the silica, right down to the particle scale. Among other things, they were able to see that the vaccine had a tendency to clump within the silica, making it less effective.
“Now we know what makes the vaccine less effective, and how to optimize it. We know exactly how much vaccine should be put in the silica capsule for it to work best in the body and the clinical trials can be better interpreted,” explains Bordallo.
Goodbye, needles and refrigeration
The vaccine is particularly promising for developing nations, explains the study’s other main author, Martin K. Rasmussen, a former student at the Niels Bohr Institute and current doctoral student at the Technical University of Denmark.
“Getting rid of needles being poked into the arms of little children is an advantage in and of itself. It also eliminates any need to sterilize needles and possible side effects such as swelling and infection. And, unlike the vaccine in use today, this type of vaccine needn’t be refrigerated. As such, costs will be reduced and the vaccine’s administration will be eased,” he says.
The researchers hope that the 3D technology will also help develop oral vaccines against several other types of disease. The goal of the Danish researchers’ Brazilian collaborative partners is to produce a six-in-one oral vaccine against diphtheria, tetanus, whooping cough, polio, Hib, and hepatitis B. The vaccine against diphtheria and tetanus is already being developed.
The researchers conducted the study in collaboration with the Institute of Physics at the Universidade de São Paulo, Brazil; Virology Laboratory, Butantan Institute, Brazil; Immunochemistry Laboratory, Butantan Institute, Brazil; the Technical University of Denmark; Helmholtz Center Berlin for Materials and Energy, Germany; Paul Scherrer Institute, Switzerland; ESRF-The European Synchrotron, ID16B, France and the European Spallation Source, Sweden.
Funding for the research came from Danscatt; São Paulo Research Foundation, FAPESP; European Synchrotron Radiation Facility, France; Federal Ministry of Education and Research, Germany.
Source: University of Copenhagen