New research shows how H. pylori, a potentially pathogenic bacterial species that infects half the people on Earth, establishes its niche.
The stomach-dwelling bacteria Helicobacter pylori survives in the stomach—a hellish, churning vat of hydrochloric acid—by holing up inside that organ’s pitlike glands and establishing squatter’s rights. Once the germ has set up shop, the investigators learned, even competing strains of the same species can’t displace it, or even share its hideout.
The findings, published in PLOS Biology, raise questions about the effectiveness of probiotic approaches, in which people ingest “good” germs in an effort to supplant “bad” germs. Yet the findings also hint at possibly effective ways to deal with the potentially life-threatening H. pylori strains.
“This study changes the way we think about how microbes like H. pylori establish their chronic persistence in the body,” says senior author of the study Manuel Amieva, associate professor of pediatrics and of microbiology and immunology at the Stanford University School of Medicine. The lead author is former graduate student Connie Fung.
Perks and dangers of H. pylori
H. pylori is the primary cause of stomach ulcers and stomach cancer. Fortunately, the great majority of infected people remain asymptomatic throughout their lives: Only 10-15 percent of infected people get ulcers, and only 1 percent get stomach cancer.
Plus, there are reasons for thinking that infection by H. pylori, which has co-existed with humans since the earliest days of our species, may have some advantages. For instance, H. pylori infection is associated with lower incidences of asthma and other allergies. The combination of that upside and the low-incidence, high-impact nature of H. pylori’s adverse effects gives pause to medical researchers considering ways of preemptively eradicating it from all of our stomachs. It may be wiser to substitute friendlier “designer” strains.
But that won’t be easy, the study shows.
Hang-out spots
From an ecological point of view, H. pylori has succeeded where practically every other bacterial pest has failed. It has evolved the capacity to persist for prolonged periods—often for a person’s entire life—in the stomach, whose intense acidity, swiftly shifting chemical contents and rapid cellular turnover make it one of the harshest environments a microbe encounters.
Although H. pylori is susceptible to antibiotics, it’s not uncommon for these drugs to fail to completely clear the stomach of the microorganism. “The re-emerging strain is invariably just the same as the one thought to have been eradicated,” Amieva says, suggesting the presence of some niche where H. pylori can find refuge and replenish its numbers in safety. But exactly how has been unclear.
H. pylori is a corkscrew-shaped microbe equipped with a tuft of spinning, hairlike projections called flagella that enable it to swim freely in an aqueous liquid medium or to bore into viscous fluids. Microbiologists have long thought it avoids being dissolved in a sea of stomach acid by hiding out in the mucus layer that lines the stomach and protects the digestive organ from being eaten by the acid it produces.
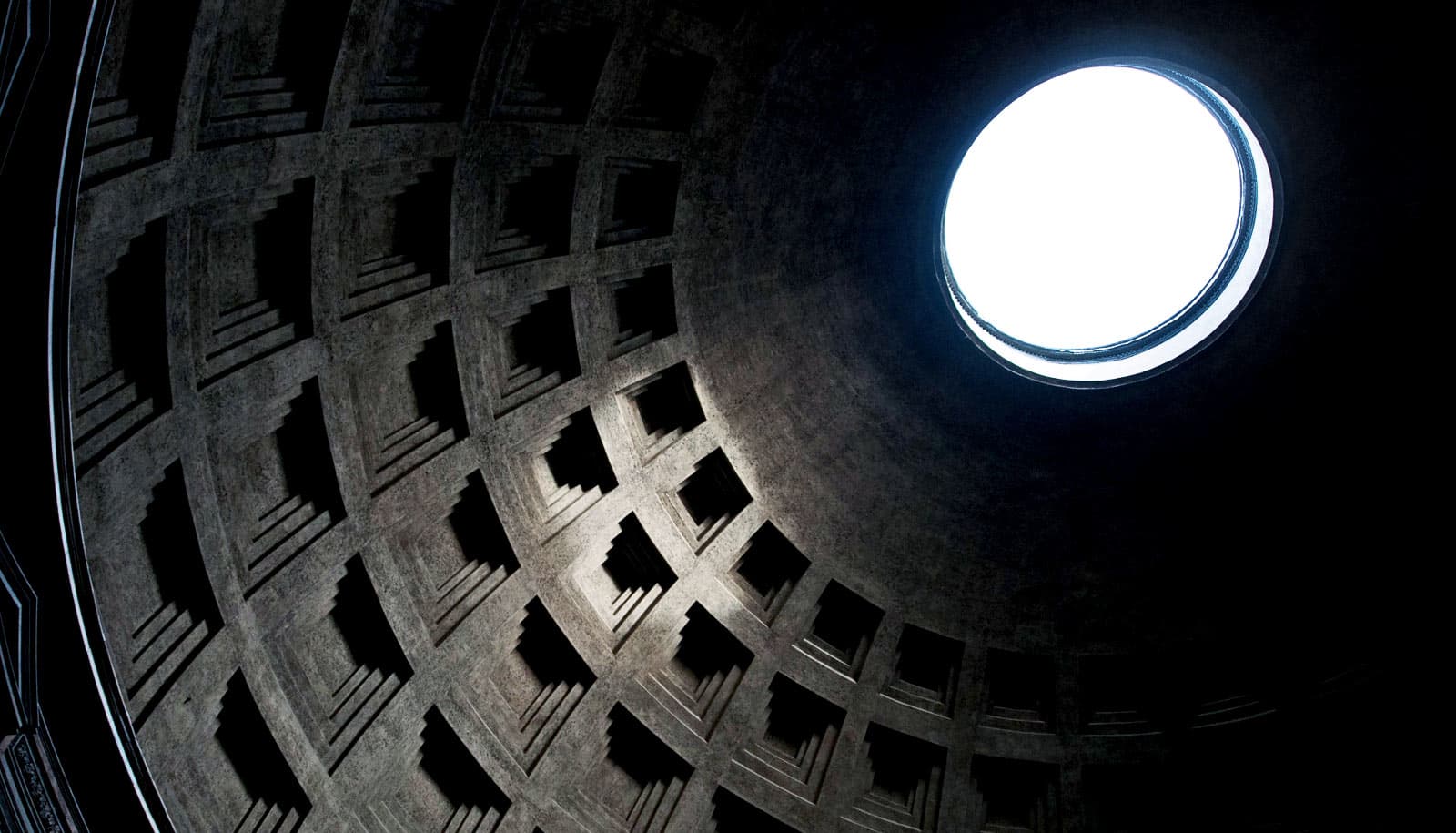
Little pits
That’s part of the story. But the new study reveals a safer survival tactic for the bug: steering itself into one of the myriad pitlike glands that dot the stomach’s inner surface and, afterward, fending off all comers.
In a study published in 2015, Amieva’s group discovered the presence of H. pylori within stomach glands. But why the microbe would choose to hang out there was not obvious.
The new study, Amieva says, shows that once a particularly hardy, or lucky, individual H. pylori bacterium manages to colonize a gland, the resulting “founder” strain becomes extremely difficult to dislodge even by members of an essentially identical strain, for reasons that remain mysterious but may have to do with the fact that each gland has only a single, tiny entry point.
Color-coded bacteria
The researchers inoculated mice’s stomachs with two versions of an otherwise identical H. pylori strain, differing only in that one group had been genetically modified so it emitted fluorescent green light when stimulated by a laser, while the other group was modified to glow red. Later, the scientists could observe the different-colored strains’ success in establishing themselves within glands along the length of the mice’s stomachs.
The scientists used a form of microscopy that allowed them to move their focus through successive depths of intact tissue rather than view separate thin tissue slices. They also used a technique called CLARITY that renders tissues transparent without destroying their microanatomical integrity. That combination let them visualize, in three dimensions, H. pylori’s presence along the depths of the stomach glands.
Instead of mixing randomly—as one would expect if occupancy of a gland by one “color” of bugs presented no barrier to entry by the other color—the two sets of H. pylori occupied distinct patches of stomach-surface area, indicating an exclusive “first-come, first-served” advantage for a given gland’s initial occupant and further suggesting that, having established itself within a gland, a “red” or “green” H. pylori strain sends forth individual progeny to adjacent glands in which they plant their flags, thrive, exclude newcomers, multiply, and eventually release new single-celled troops to repeat the gland-by-gland expeditionary advance.
How to evict them?
This study changes the way we think about how microbes like H. pylori establish their chronic persistence in the body.
It’s still not clear precisely which tools the bacteria need to establish squatter’s rights in a gland. But when the scientists inoculated mouse stomachs with mutant H. pylori lacking the functioning chemical sensor machinery that guides its swimming direction, the bugs were unable to maintain exclusive colonies in glands.
This raises the issue of how to eradicate potentially pathogenic bacterial strains ensconced in our bodies or how to replace them by others that are less pathogenic. Probiotics have not demonstrated much success in achieving that goal yet, Amieva says.
“It’s not enough to find a good probiotic strain that can survive in the organ you want it to live in,” he says. “You need to create space for it.”
One potential approach, Amieva suggests, would be to find some way to draw the bacteria out of their protective hideouts before treating them and then replace them with a less-virulent strain.
Additional researchers from Stanford; the University of California, Davis; and the Wellcome-Sanger Institute in England also contributed to the study.
Funding came from the National Institutes of Health, the National Science Foundation, the American Gastroenterology Association, a Morgridge Faculty Scholar Award, and the Wellcome Trust. Stanford’s departments of pediatrics and of microbiology and immunology also supported the work.
Source: Stanford University