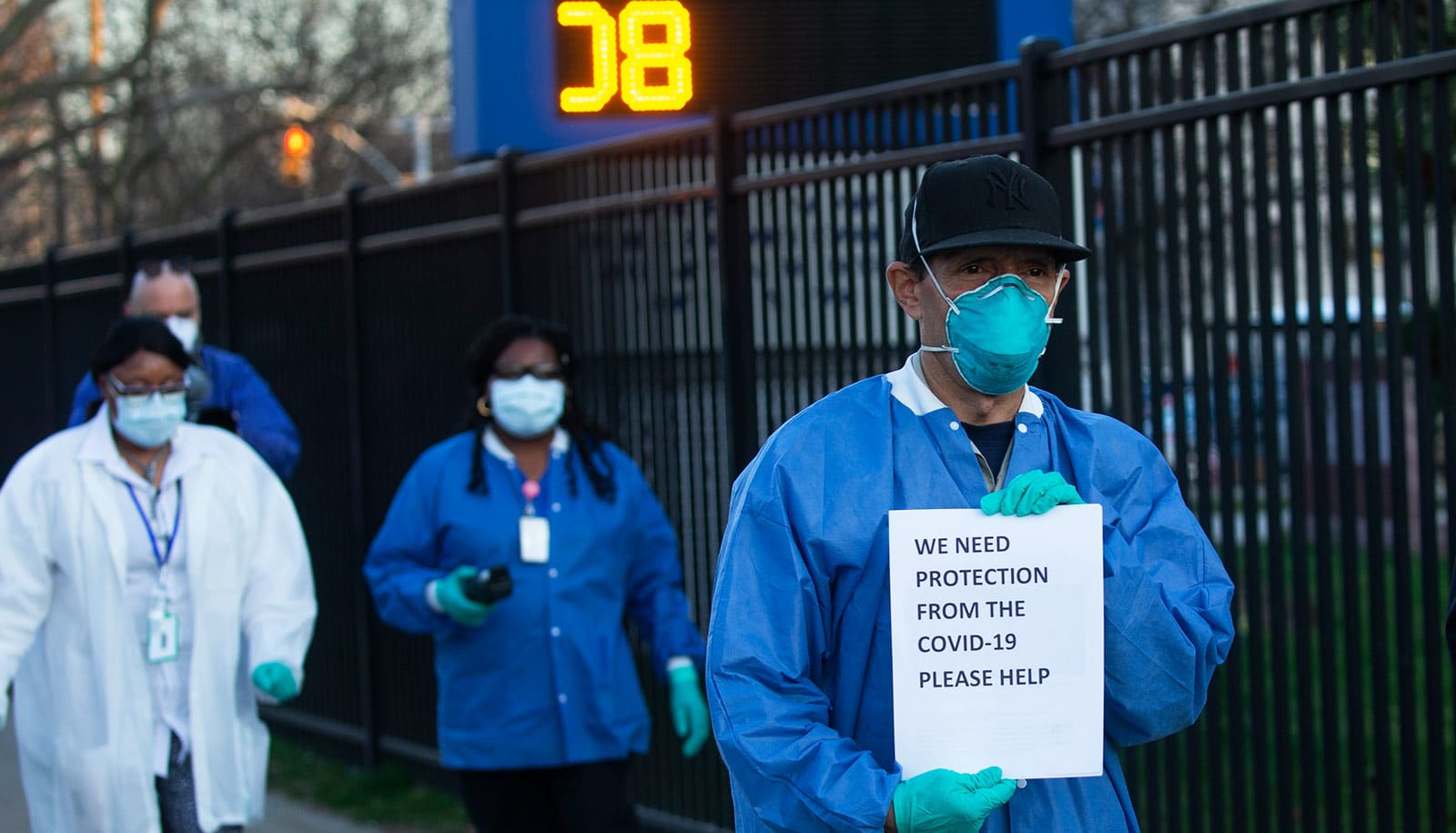
COVID exacted a huge toll on the well-being of health care workers, a new survey shows.
Already struggling with high levels of emotional exhaustion going into the pandemic, the problem grew even worse after two years of managing the crisis. Nurses have been especially hard hit.
Researchers conducted surveys over three years with more than 30,000 health care workers—including doctors, nurses, clinical social workers, administrators, and others—to track the emotional impact of the pandemic.
Their findings are published in JAMA Network Open.
Across all roles, the researchers found increases in emotional exhaustion—a way of measuring burnout and well-being—from 32% in 2019, before COVID hit, to 40% by January 2022.
“Emotional exhaustion is essentially a way of measuring a person’s ability to ‘do stuff,'” says lead author Bryan Sexton, director of the Duke University Center for Healthcare Safety and Quality. “So as the health care workforce well-being takes a hit, so does the ability to ‘do stuff’ for their patients.”
Sexton and colleagues conducted the cross-sectional survey of 30,000 healthcare workers at 76 geographically dispersed hospitals around the United States. They administered the surveys before the pandemic (September 2019) and twice during the pandemic (September 2021 and January 2022).
The survey covered safety culture and workforce well-being and engagement, plus emotional exhaustion metrics that captured both individual perceptions and the workplace climate.
The surveys asked participants to rate their agreement with statements such as: “I feel frustrated by my job,” and “Events in this work setting affect my life in an emotionally unhealthy way.”
To assess the workplace more broadly, participants rated externally focused statements, including: “People in this work setting feel frustrated by their jobs,” and “Events in this work setting affect the lives of people here in an emotionally unhealthy way.”
Nurses had the highest levels of emotional exhaustion. They started the pandemic with 41% reporting emotional exhaustion, escalating to 46% the first year and to 49% the second. This same pattern emerged for every other health care job role, albeit with lower starting rates.
Physicians were the exception.
Doctors had a unique trajectory, reporting an emotional exhaustion rate before the pandemic at 32% and actually logging a decline to 28% the first year of the pandemic. It then shot to 38% the second year.
Workloads for many physicians declined during the first year of the pandemic, as clinical appointments were cancelled and replaced in many instances with telehealth visits, which doctors could conduct from home, Sexton says. Then the onset of the Delta variant, followed by the Omicron variant, was associated with a sharp increase in workload and physician exhaustion.
The findings could be used to help guide health care employers and providers to establish more effective wellness programs, the researchers say.
“Many institutions prior to the pandemic considered themselves progressive if they had convened a task force to examine health care worker burnout,” Sexton says. “We now know that burnout is a parallel pandemic that will be felt for many years to come.
“Leaders need tiered options for responding to this issue, and we suggest that there is a need for both institutional and individual resources for health care well-being, as evidenced by the role-specific findings reported in our study.”
The National Institutes of Health and the Health Resources and Services Administration funded the work.
Source: Duke University