Repeated bacterial infections can add up over time, eventually leading to severe inflammatory disease, a new study suggests.
Small bacterial infections, which may go unnoticed and which clear the body without treatment—such as occurs in mild food poisoning—can start a chain of events that leads to chronic inflammation and life-threatening colitis.
The new findings also may identify the long-mysterious origins of inflammatory bowel disease (IBD).
Tracing inflammation’s origins
“We have discovered an environmental and pathogenic origin of chronic intestinal inflammation in the course of modeling human food poisoning as it occurs repeatedly over the adult lifespan,” explains coauthor Jamey Marth, director of the University of California, Santa Barbara’s Center for Nanomedicine and also a professor at the Sanford Burnham Prebys (SBP) Medical Discovery Institute in La Jolla, California.
“Remarkably, salmonellae have figured out a way to disrupt a previously unknown protective mechanism in the gut that normally prevents intestinal inflammation,” she explains.
“Such a discovery might explain the origins and mechanisms responsible for human colitis and IBD.”
A breakthrough eight years in the making, the research began as an investigation into the origin of chronic inflammatory diseases spanning colitis and IBD.
The group’s radically different hypothesis took shape from a few possible clues, starting with increasing evidence that the genetic makeup of an individual plays a limited role in common inflammatory diseases, including colitis and IBD. Twins show relatively small concordance for both developing IBD, for example. Such findings implicate unknown environmental factors in disease origins.
Noting that studies from other laboratories had reported seasonal bacterial infections in humans were correlated with increased diagnoses of IBD, the investigators hypothesized that recurrent low-grade bacterial infections may trigger the onset of chronic inflammation.
“Trying to determine the origin of a disease is important as it often indicates more rational and effective preventions and treatments,” Marth says.
The damage done
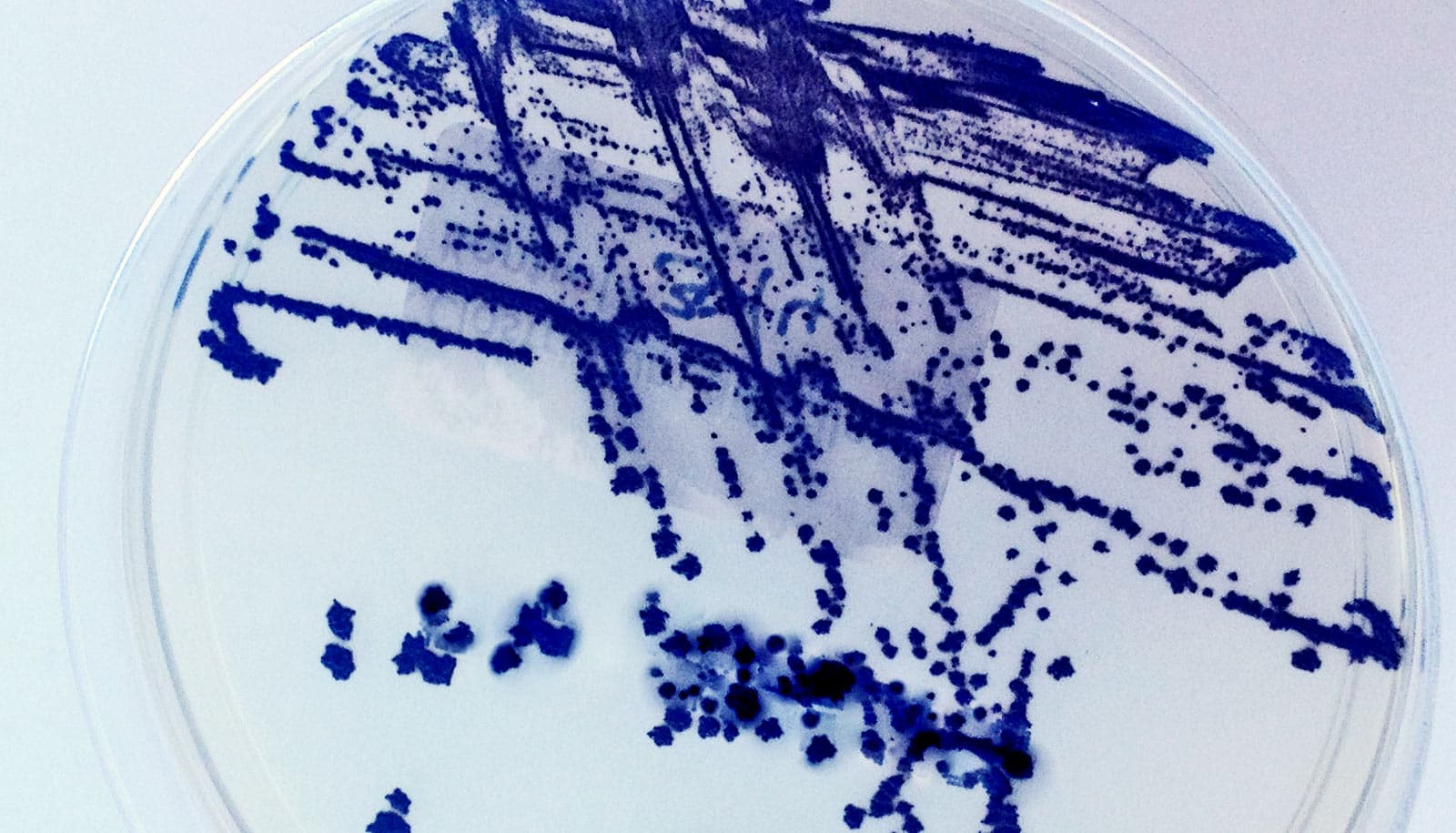
The researchers developed a model of mild human food poisoning using healthy mice that they gave a very low dose of a common bacterial strain, Salmonella typhimurium, which is widespread throughout the environment and is a leading cause of human foodborne illness and disease. Most often, the result is temporary intestinal discomfort and dysfunction.
The majority of these infections are likely unreported, which suggests the numbers of infections among individuals over a lifespan is greatly underestimated.
“We investigated whether low-titer and nonlethal salmonella infections of mice—designed to model repeated episodes of human food poisoning—might lead to cumulative and chronic intestinal inflammation,” explains Michael Mahan, a professor in molecular, cellular, and developmental biology department at UC Santa Barbara. “Such a discovery might explain the origins and mechanisms responsible for human colitis and IBD.”
“This type of study had never been done before and the results were shocking…”
The team experimented with a dose of salmonella that was low enough to ensure no significant symptoms or death but that allowed the host to successfully eliminate the pathogen. By the fourth infection—months apart from the first—the inflammation had steadily increased and colitis was now present in all subjects.
Surprisingly, the disease did not improve despite the cessation of repeated infections, indicating that the damage was already done.
“This type of study had never been done before and the results were shocking,” says lead author Won Ho Yang, who holds joint appointments at UC Santa Barbara’s Center for Nanomedicine and the SBP Discovery Institute. “We observed the onset of a progressive and irreversible inflammatory disease caused by previous infections. That was quite surprising because the pathogen had been easily and rapidly eliminated by the host.”
The investigation linked the disease mechanism to an acquired deficiency of intestinal alkaline phosphatase (IAP), an enzyme produced in the duodenum of the small intestine. Salmonella infection elevated neuraminidase activity in the small intestine, which in turn accelerated the molecular aging and turnover of IAP, resulting in IAP deficiency in the colon.
IAP is important because its job is to remove phosphates from molecules such as pro-inflammatory lipopolysaccharide (LPS)—produced by various resident bacteria in the colon—thereby transforming LPS from a toxic to a nontoxic state. In fact, published studies by others have recently reported IAP deficiencies and high neuraminidase levels in IBD patients.
Bad news, good news
“Our findings are of potential great concern to the human population,” Marth says. “Food contamination at these low bacterial levels is likely to be more common than we recognize, while symptoms could be nonexistent or mild and disappear in a day or two without treatment.”
Higher anxiety risk for people with I.B.D.
“Repeated over time, we find that such minor infections are sufficient to trigger disease months and perhaps years later, depending upon the number and timing of infections an individual has experienced over his or her lifetime,” she explains.
“There is an unexpected additive effect of previous infections in the likelihood of developing colitis. This environmental factor may be responsible for triggering disease among some segments of the human population,” Marth adds.
The good news is that ways to boost IAP levels or inhibit neuraminidase already exist. IAP augmentation is as simple as adding the enzyme to drinking water. A marketed antiviral neuraminidase inhibitor, a drug used to prevent influenza viral infections, can inhibit neuraminidase.
“This opens a new door where these therapies could be easily applied and tested,” Mahan notes. “We found that both treatment approaches were similarly effective at preventing the onset of disease.”
Could soy protein ease irritable bowel diseases?
The researchers report their findings in the journal Science.
Additional researchers collaborating on the research are from UC Santa Barbara, UC San Diego, and Ludwig-Maximilian University of Munich.
Grants from the National Institutes of Health’s National Heart, Lung, and Blood Institute funded the research. The Wille Family Foundation and by the German Research Foundation provided additional support.
Source: UC Santa Barbara