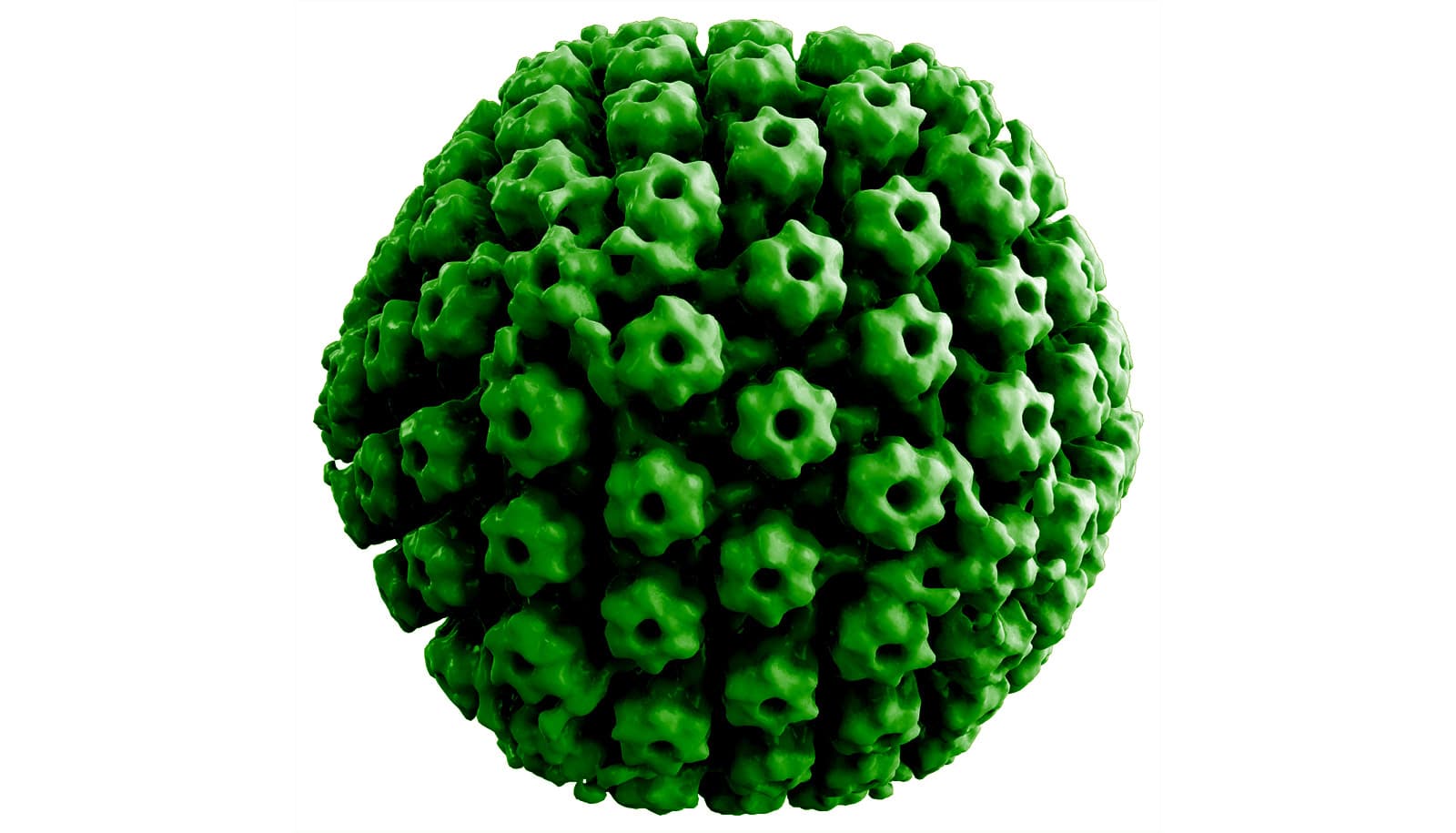
New research shows that the Epstein-Barr virus, a common type of herpes virus, triggers multiple sclerosis by priming the immune system to attack the body’s own nervous system.
Scientists have long suspected—but failed to prove—a link between certain viral infections and the development of multiple sclerosis, a crippling autoimmune disease that affects nearly 1 million Americans.
The study, published in Nature, shows that approximately 20% to 25% of patients with multiple sclerosis have antibodies in their blood that bind tightly to both a protein from the Epstein-Barr virus, called EBNA1, and a protein made in the brain and spinal cord, called the glial cell adhesion molecule, or GlialCAM.
“Part of the EBV protein mimics your own host protein—in this case, GlialCAM, found in the insulating sheath on nerves,” says William Robinson, professor of immunology and rheumatology at Stanford University School of Medicine. “This means that when the immune system attacks EBV to clear the virus, it also ends up targeting GlialCAM in the myelin.”
Myelin forms the protective coating around nerve cells, and when it’s damaged, electrical impulses can no longer jump efficiently from one nerve to the next, resulting in the numbness, muscle weakness, and severe fatigue of multiple sclerosis.
“This is the first time anyone has shown rather definitively that a virus is the trigger for multiple sclerosis,” says coauthor Lawrence Steinman, professor of neurology. “And these exciting findings open up some new directions for clinical trials in MS treatment.”
Making the connection
Previous research has shown that multiple sclerosis patients have increased antibodies to a variety of common viruses, including measles, mumps, varicella-zoster, and Epstein-Barr virus. In fact, more than 99% of MS patients have EBV antibodies in their blood, indicating a prior infection, compared with 94% of healthy individuals. But despite this epidemiologic correlation, scientists have struggled to prove a causal connection.
“Nobody really knows what causes autoimmune diseases, and for many decades, all sorts of different viruses have been hypothesized,” Robinson says. “But when people did further mechanistic digging, everything fell apart, and it turned out that getting those other viruses didn’t actually cause MS.”
To search for this elusive mechanistic link, the researchers started by examining the antibodies produced by immune cells in the blood and spinal fluid of nine MS patients. Unlike in healthy individuals, the immune cells of MS patients traffic to the brain and spinal cord, where they produce large amounts of a few types of antibodies. Patterns of these antibody proteins, called oligoclonal bands, are found during analysis of the spinal fluid and are part of the diagnostic criteria for MS.
“No one knows exactly what those antibodies bind to or where they’re from,” Robinson says. “So the first thing we did was analyze the antibodies from the oligoclonal bands, and showed that they come from B cells in the spinal fluid.”
B cells are a type of white blood cell made in the bone marrow, and the technology to sequence these cells individually was developed by the Robinson lab about eight years ago. “In the past, researchers would take serum and spinal fluid from MS patients and test them on planar arrays or throw them on histology slides to see what sticks,” says research scientist Tobias Lanz, a coauthor of the study.
“What we did was a different approach: We took B cells from the spinal fluid, single-cell sorted them and sequenced each one separately. In a single-cell format and at the scale of tens to hundreds of B cells per patient, that had not been done before.”
Epstein-Barr virus and multiple sclerosis
Once the researchers determined that the oligoclonal bands in MS are produced by the sorted B cells in the spinal fluid, they expressed individual antibodies from these cells and tested them for reactivity against hundreds of different antigens.
“We started with human antigens,” Robinson says, “but couldn’t find clear reactivity. So eventually we tested them against EBV and other herpes viruses, and lo and behold, several of these antibodies, and one in particular, bound to EBV.”
Six of the nine MS patients had antibodies that bound to the EBV protein EBNA1, and eight of nine had antibodies to some fragment of EBNA1. The researchers focused on one antibody that binds EBNA1 in a region known to elicit high reactivity in MS patients. They were then able to solve the crystal structure of the antibody-antigen complex, to determine which parts were most important for binding.
Before this discovery, Robinson says he’d been unconvinced that EBV caused MS. “We all thought it was just kind of an artifact; we didn’t really think it was causative. But when we found these antibodies that bound EBV in the spinal fluid, produced by the spinal fluid B cells, it made us revisit the potential association that we’d dismissed.”
Molecular mimicry
Next, the researchers tested the same antibody on a microarray containing more than 16,000 human proteins. When they discovered that the antibody also bound with high affinity to GlialCAM, they knew they’d found a specific mechanism for how EBV infection could trigger multiple sclerosis.
“EBV tricks the immune system into responding not only to the virus, but also to this critical component of the cells that make up the white matter in our brains,” Steinman says. “To use a military metaphor, it’s like friendly fire: In fighting the virus, we damage our own army.”
To find out what percentage of MS might be caused by this so-called “molecular mimicry” between EBNA1 and GlialCAM, the researchers looked at a broader sample of MS patients and found elevated reactivity to the EBNA1 protein and GlialCAM in 20% to 25% of blood samples in three separate MS cohorts.
“Twenty-five percent is a conservative number,” Robinson says, noting that it doesn’t include patients who may have previously reacted to GlialCAM following EBV infection but whose immune response has evolved since the initial trigger.
In fact, a study of 801 MS cases from more than 10 million active-duty military personnel over 20 years found that EBV infection was present in all but one case at the time of MS onset. A paper describing that study, published this month in Science, found that of 35 people who were initially EBV-negative, all but one became infected with EBV before the onset of MS. In addition, this separate group of researchers identified the same EBNA1 region as a major antibody target in MS patients. Together with the discovery of EBNA1/GlialCAM cross-reactivity, this data provides compelling evidence that EBV is the trigger for the vast majority of MS cases, as Robinson and Steinman point out in a Science Perspective, also published in January.
Mouse models
In work guided by coauthor and senior research scientist Peggy Ho, the importance of the anti-EBNA1 immune response was further assessed by using a common mouse model of MS called experimental autoimmune encephalomyelitis. After receiving an injection of a fragment of the EBNA1 protein, the mice exhibited more severe paralysis, more immune cells invading their central nervous system, and more damage to the protective coating on their nerve cells, compared with mice injected with a control protein fragment.
“It’s just further connecting the dots,” Robinson says. “If you immunize a mouse with a particular antigen and it makes paralysis worse, it suggests that an immune response against that target can contribute to MS pathogenesis.”
Future MS treatments?
Perhaps the most exciting aspect of this discovery is its potential to create new pathways for the clinical treatment of multiple sclerosis. “If a virus is the target of the immune response that’s going an unwanted way in the MS brain, why not get rid of the virus?” Steinman says, noting that a vaccine against Epstein-Barr virus could perhaps eventually eradicate MS, in the same way polio was eradicated from the United States in the 1970s.
But this research also demonstrates why manufacturers would need to be extra careful in selecting which antigens to incorporate into an EBV vaccine. “You don’t want to choose those antigens, like EBNA1, that could cause autoimmunity,” Lanz says.
In addition, an EBV vaccine wouldn’t necessarily help patients who have already developed EBNA1/GlialCAM cross-reactivity. For those patients, a better option might be to “tolerize” the immune system so it no longer responds to GlialCAM, Steinman says. “There are two promising technologies here, one involving a reverse vaccine using DNA plasmids and another using RNA technology from the same company in Germany that made the Pfizer vaccine for COVID-19.”
The discovery of how EBV triggers multiple sclerosis could also have ramifications for research into other autoimmune diseases, such as lupus and rheumatoid arthritis, which, like MS, have been significantly associated with EBV infection in epidemiologic studies.
Researchers from the University of Heidelberg, Germany; the Howard Hughes Medical Institute; UC San Francisco; the NYU Grossman School of Medicine; the SLAC National Accelerator Laboratory; the Institute of Experimental Immunology in Lubeck, Germany; Atara Biotherapeutics Inc.; and the University of Oxford, UK, also contributed to the work.
Funding for the work came from the National Institutes of Health, the Juvenile Diabetes Research Foundation, the Lupus Research Alliance, the German Research Foundation, Atara Biotherapeutics Inc., the NYU Grossman School of Medicine, and the US Department of Energy.
Source: Hadley Leggett for Stanford University