A new technique may simplify the placement of electrodes in the brains of patients with epilepsy.
The method, called BrainGuide, is a software-based automation tool for use by neurosurgeons that plots the correct placement of probes in the brains of patients with non-treatable forms of epilepsy.
The gathered information could then be used to design future procedures in which doctors could remove, destroy with lasers, or modulate with electrical stimulation the portion of the brain causing the seizures.
Nitin Tandon, a professor of neurosurgery at the University of Texas Health Science Center at Houston (UTHealth), director of the epilepsy surgery program at Memorial Hermann-Texas Medical Center, and an adjunct professor of electrical and computer engineering at Rice University who helped a team of students create the new technique, hopes to ease the burden on doctors who take the long way around when planning brain implants for a single patient before the initial operation.
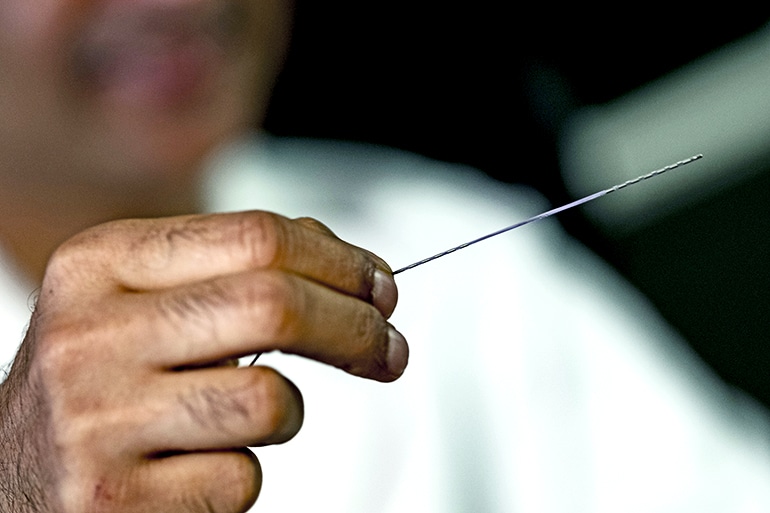
“Doctors want to make sure they’re targeting the right part of the brain,” says team member Alex Gardner. “They do that by implanting these long, thin probes that are lined with electrodes, which then record over the course of several weeks, and they gather data.”
“Our part of the problem was figuring out exactly where to put those,” he says. “Doctors currently spend several hours planning each surgery individually. They look at all the data and based on their knowledge of what the brain looks like and the patient’s vasculature, the doctors decide what to do. We also need to avoid regions that are very dense and have a lot of blood in them.”
“The hope is someday, when we’ve had enough of a patient cohort and refined this technique further, this could save us a lot of time,” Tandon says.
The students, all senior computational and applied mathematics majors, used MRI and CT data from 40 of Tandon’s patients to build models of each brain and decide where the probes should go, working with Rice alumnus Kiefer Forseth, a researcher in Tandon’s lab.
Each patient can have up to 256 electrodes on up to 20 probes—thin, plastic-encased wires that must not only avoid vessels but also cross the brain regions of epileptic interest, Gardner says.
With the proper data, the students say the program can predict optimum electrode implantation in about 30 seconds and with a higher degree of safety than previous methods.
“It’s ideal if we find trajectories that are perpendicular to the skull, because they’re easier to screw and more likely to follow the trajectory that we prescribe,” Gardner says. “That weighs in almost as heavily as the vasculature does.”
A.I. spots epilepsy seizures in advance
Having completed their part, the project now moves back to UTHealth for more validation, the students say.
“They need to validate and optimize this on a larger patient set moving forward, double check its accuracy and to compare it with previous surgeries,” says team member Wendy Knight.
“Obviously this work is a start, and there’s a lot more that needs to be done,” Tandon adds. “What’s missing is that it is currently driven by what I have done before, which may not necessarily be what some other surgeon wants to do, so we want to create a template that works for any surgeon.”
Student Evan Toler also worked on the project.
Source: Rice University