Drug-resistant bacteria can gang up on us, research finds, and trying different antibiotics to control a “superbug” may only encourage others lurking nearby.
It’s time to think about such bacteria as members of an antibiotic-resistant ecosystem in health care environments—not as single species that act and respond alone—say University of Michigan researchers.
Their new findings come from a study of hundreds of nursing home patients.
Forty percent of the 234 frail elderly patients in their study had more than one multidrug-resistant organism, or MDRO, living on their bodies. Patients who had specific pairs of MDROs were more likely to develop a urinary tract infection involving an MDRO.
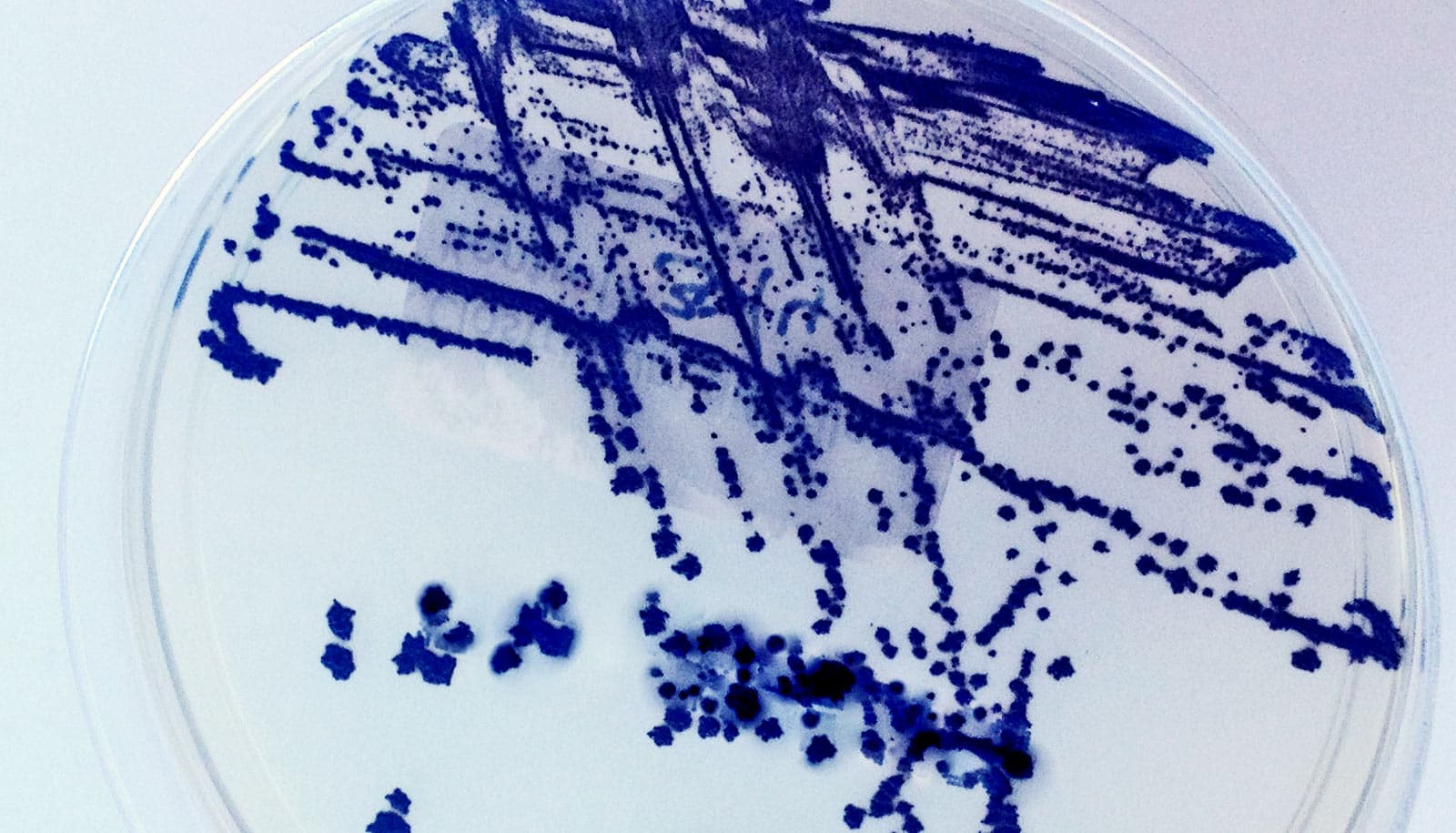
The researchers created a map of interactions among bacteria and classes of antibiotics, which they’ve published with their findings in the Proceedings of the National Academy of Sciences.
Eventually, that kind of mapping could help health care providers. For instance, they could choose to treat a patient with a specific antibiotic not just because of its ability to kill one MDRO, but also for its potential downstream impact on other MDROs that may be lurking on the patient, or nearby.
But that will take time, and more research in the laboratory and in health care facilities, say the researchers, led by systems biologist Evan Snitkin of the University of Michigan Medical School department of microbiology and immunology.
So in the meantime, they hope their new findings will give healthcare providers and patients even more reason to avoid using antibiotics in the first place unless they’re truly necessary—because “superbugs” evolve in response to them.
It’s an ecosystem
The researchers used detailed data from a long-term study of nursing home patients led by geriatrician Lona Mody, professor of internal medicine, who studies infection transmission and prevention in nursing homes.
Nearly two-thirds of the patients studied received one or more of 50 different antibiotics during the study period. All the patients in the study used a urinary catheter to empty their bladders for at least three days during the study period. This allowed the researchers to look at patterns of urinary tract infections, which in nursing home and hospital patients often arise from bacteria entering the bladder along a catheter.
The findings showed that colonization of such patients’ skin, noses, and throats with common MDROs was not random.
This blood test could fight antibiotic-resistance
“We observed a complex network of interactions, with acquisition of each of six different MDRO species being influenced by different sets of antibiotics, and primary MDRO colonization in turn increasing the risk of acquisition and infection by other MDROs,” says lead author Joyce Wang, a postdoctoral fellow in Snitkin’s lab who led the analysis.
Colonization with one MDRO increased the risk of acquiring other MDROs—but not all others. It was as if they were interacting very specifically with other species. And treatment of a patient with any given antibiotic increased their chances of being colonized with an MDRO—which in turn altered their risk of becoming colonized with another MDRO later.
The worst offenders
The researchers focused on two of the most dangerous MDROs—vancomycin resistant Enterococcus (VRE), and methicillin-resistant Staphylococcus aureus (MRSA)—as well as four Gram-negative bacteria that have evolved resistance to two powerful antibiotics.
One of the four, Proteus mirabilis, causes many catheter-associated UTIs and can form biofilms that involve many bacteria. It’s known to release a compound called urease, which acts as a means of communication among bacteria. The other three species of MDRO studied were Acinetobacter baumannii, Escherichia coli, and Pseudomonas aeruginosa.
This trio of antibiotics gangs up to kill superbugs
These same species are known to cause many infections in hospitals, which have poured major effort into fighting them and preventing their spread.
“A lot of the attention in infection prevention is paid to large academic hospitals—but this is a fruitless endeavor if you’re not controlling the same organisms in all the connected health care facilities and nursing homes,” Snitkin says. “We need to understand what clinical practices drive the spread of MDROs in health care facilities, and counterintuitively, it appears that a key factor is the use of certain antibiotics used against an individual organism that may impact other circulating organisms.”
In short, every nursing home and likely every hospital in America is home to a natural experiment in the evolution of bacteria strains, to become resistant to drugs and to survive on a host patient or travel between hosts.
The people who work to prevent infections in health care facilities could someday harness advanced DNA sequencing techniques to help them combat superbugs, Snitkin says. These tools, which he and his colleagues have been using in their research labs for a decade, help pinpoint exactly which strains of different bacteria are present, and how they’re evolving.
That, combined with knowledge about how different MDRO strains interact with one another and how specific antibiotics affect them, could help steer doctors’ decisions in future.
Funding came from the Centers for Disease Control and Prevention, and a pilot grant from the Claude D. Pepper Older Americans Independence Center, a research division of the university’s Geriatrics Center funded by the National Institute on Aging of the National Institutes of Health.
Source: University of Michigan