Researchers have discovered that accumulated DNA damage in the retina is a key contributor to age-related macular degeneration.
They also found that targeting specific retinal cell types may lead to treatments that slow or stop progression.
Affecting approximately 200,000 Americans annually, AMD is a major cause of blindness in people over 50. It exists in two forms: wet, which is treated with well-established therapies, and dry, which lacks effective remedies.
The study, which appears in the journal Aging Cell, reveals how DNA damage, a hallmark of aging, compromises the retina’s function and accelerates vision loss.
“Our findings highlight the critical role DNA damage repair plays in maintaining retina health for good vision,” says co-corresponding author Dorota Skowronska-Krawczyk, a University of California, Irvine associate professor of physiology and biophysics.
“Because age is the strongest risk factor for AMD, gaining deeper insights into the underlying biology of aging in the eye is essential for developing effective therapies.”
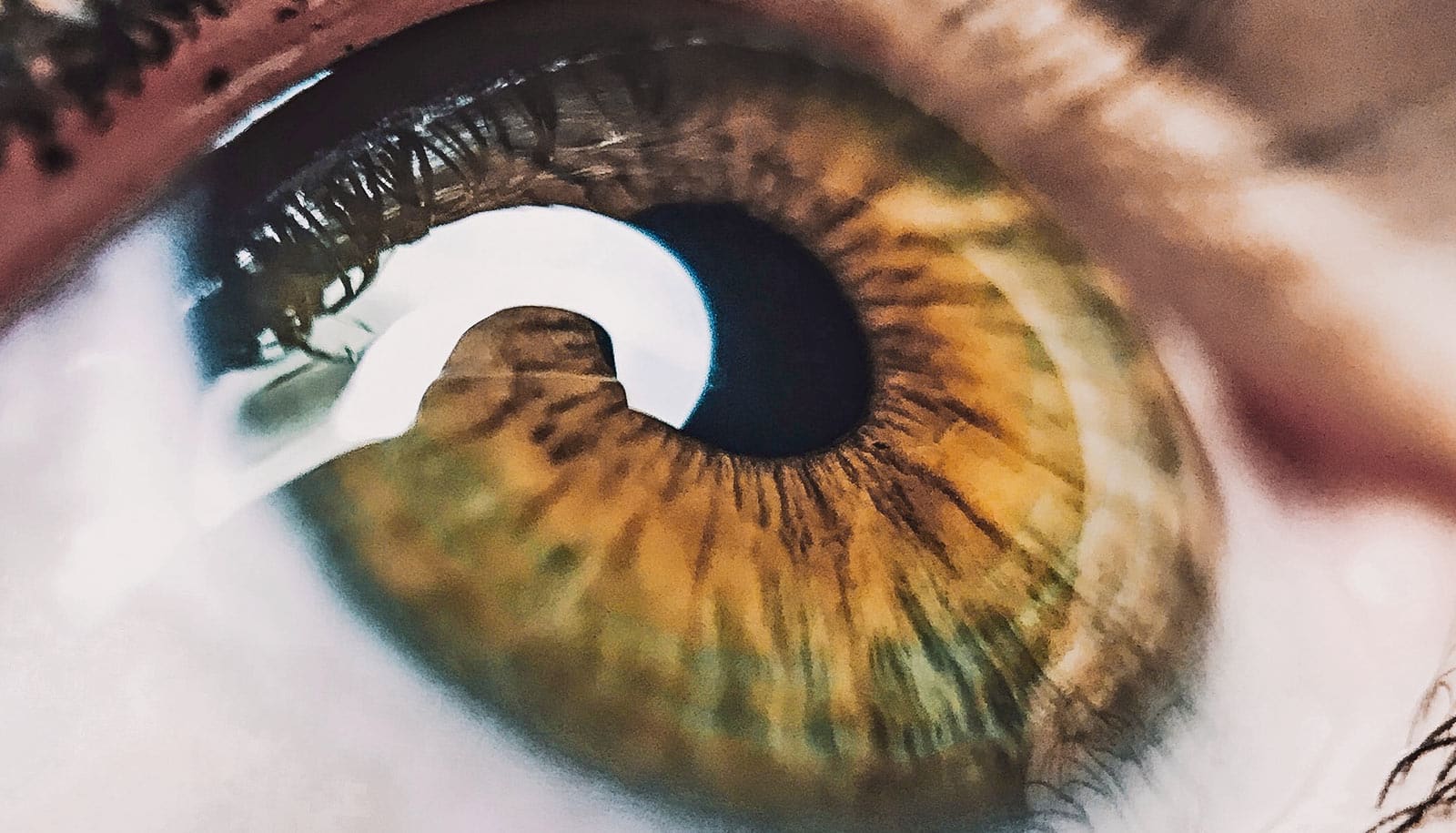
The retina, a light-sensitive tissue at the back of the eye, consumes more oxygen than any other tissue in the body and relies on the retinal pigment epithelium cell layer to function properly. Its exposure to light and intense metabolic activity makes it highly vulnerable to oxidative stress and the accumulation of DNA damage over time, a process closely linked to aging. Understanding the delicate relationship between the retina and the retinal pigment epithelium and the basic mechanism driving age-related changes is crucial for developing new approaches to combat AMD.
The team compared a mouse model with reduced levels of ERCC1-XPF, a DNA repair enzyme, with both young, healthy mice and naturally aging mice. By just 3 months of age, the model showed signs of visual impairment, structural alterations in the retina, abnormal blood vessel formation, and shifts in gene expression and metabolism, as well as mitochondrial dysfunction in the retinal pigment epithelium. All these changes mirror those seen in natural human eye aging.
“The more we know about how DNA damage contributes to eye diseases like AMD, [the better] we can develop interventions that address the root causes of vision loss. These could include strategies to counteract oxidative stress, enhance DNA repair, or even remove damaged cells before they cause harm,” Skowronska-Krawczyk says.
“We plan to investigate which cell types drive age-related changes by selectively impairing DNA mechanisms. Our goal is to advance the development of preventative interventions that significantly reduce the burden of age-related vision loss and improve the quality of life for millions.”
Additional researchers from UC Irvine, the University of Minnesota, the University of Florida, and Columbia University contributed to the work.
Support for this work came from the University of Minnesota Foundation, a generous donation from Cecilee Faster, and the National Institutes of Health.
Source: UC Irvine