Researchers have shown that personalized cancer vaccines made using DNA can program the immune system to attack malignant tumors, including breast and pancreatic cancers.
The researchers conducted the study in mice with breast cancer and one patient with late-stage pancreatic cancer.
The COVID-19 vaccines—designed using bits of genetic information that prime our immune systems to recognize and fight off viral infections—have become lifesavers in the global fight to end the pandemic.
Now, the new research has shown that a similar vaccine approach can be used to create personalized vaccines that program the immune system to attack malignant tumors, including breast and pancreatic cancers.
The tailor-made vaccines are designed to target mutated proteins called neoantigens that are unique to a patient’s tumors. Unlike the COVID-19 vaccines made by Moderna and Pfizer/BioNTech that rely on genetic material called mRNA, the personalized cancer vaccines are made using DNA.
“We took a small tissue sample from a tumor in a 25-year-old male patient with late-stage pancreatic cancer and used it to develop a personalized vaccine based on the unique genetic information in that tumor,” says William Gillanders, professor of surgery at Washington University School of Medicine in St. Louis and senior author of the paper in the journal Genome Medicine.
“We think this is the first report of the use of a neoantigen DNA vaccine in a human, and our monitoring confirms the vaccine was successful in prompting an immune response that targeted specific neoantigens in the patient’s tumor,” Gillanders says.
The study explores how techniques used to create personalized cancer vaccines can be improved to help the body unleash a more effective, longer-lasting, tumor-fighting immune response.
The findings also show that a personalized DNA vaccine coupled with other immunotherapies can generate a robust immune response capable of shrinking breast cancers in mice. While the DNA vaccine did not shrink tumors in the pancreatic cancer patient, it did produce a measurable immune response that targeted the tumor.
Gillanders, who treats breast cancer patients at Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine, says DNA vaccine platforms offer some important advantages over other personalized vaccine platforms now in early clinical trials, such as those relying on mRNA, dendritic cells, and synthetic peptides.
Because the neoantigen DNA vaccine focuses the immune response on neoantigens that exist only in tumor cells, it lowers the risk of dangerous side effects, such as damage to normal healthy tissues or the triggering of an intolerance or bad reaction to the vaccine.
“DNA vaccines are relatively easy and cost effective to manufacture compared with other neoantigen vaccine platforms such as those that use dendritic cells or mRNA, for example, making the DNA vaccine platform attractive for neoantigen vaccines,” Gillanders says. “The DNA vaccine platform also can be readily engineered to include multiple neoantigens. Additional immune modulators can also be integrated into the vaccine to increase the immune responses.”
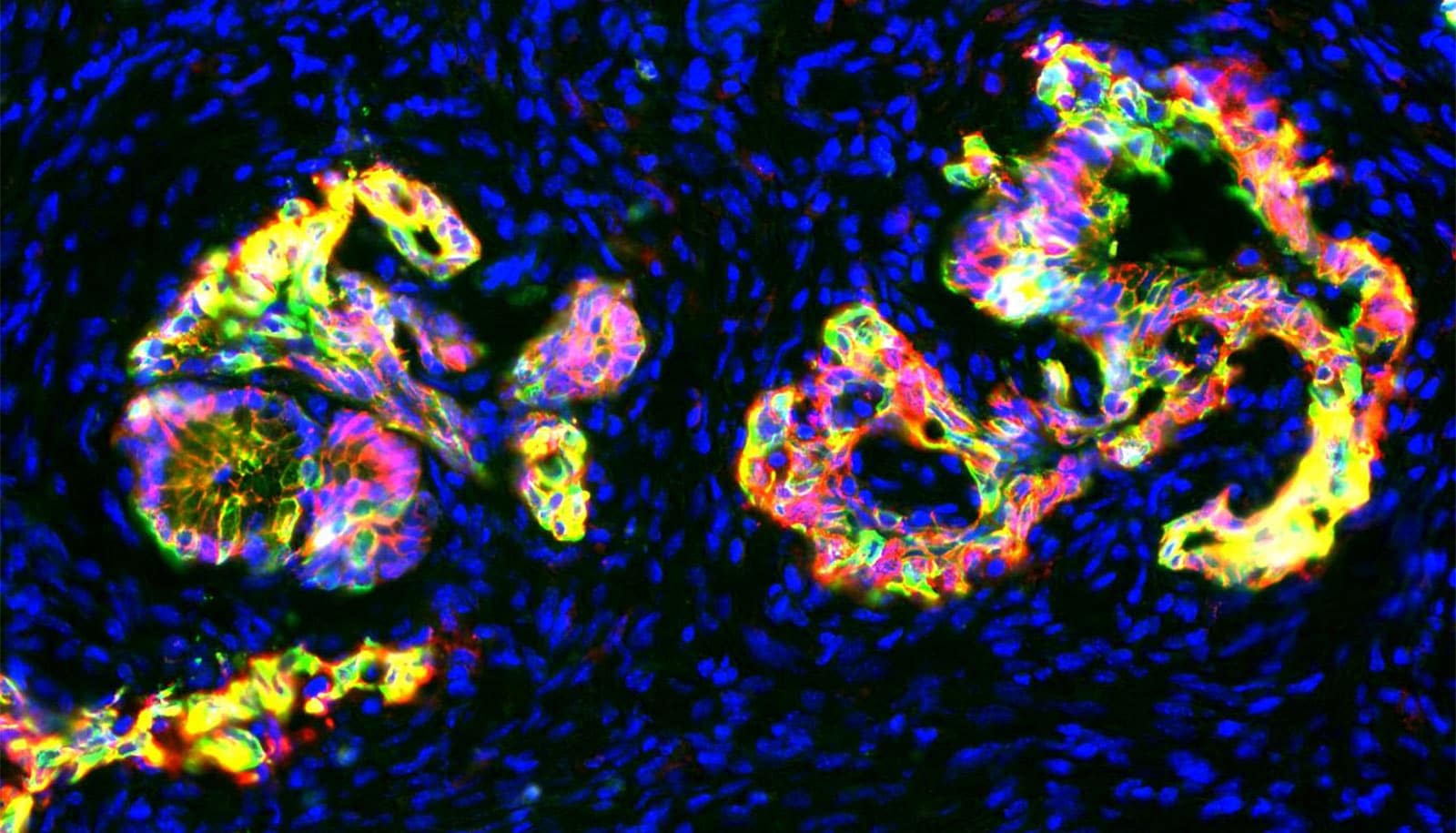
Like other personalized vaccines now under development, the DNA vaccine platform targets neoantigens, abnormal protein fragments that are created as cancerous tumor cells mutate and grow. Since each cancer generates unique mutations, each DNA vaccine is also unique and optimized to simultaneously target multiple neoantigens.
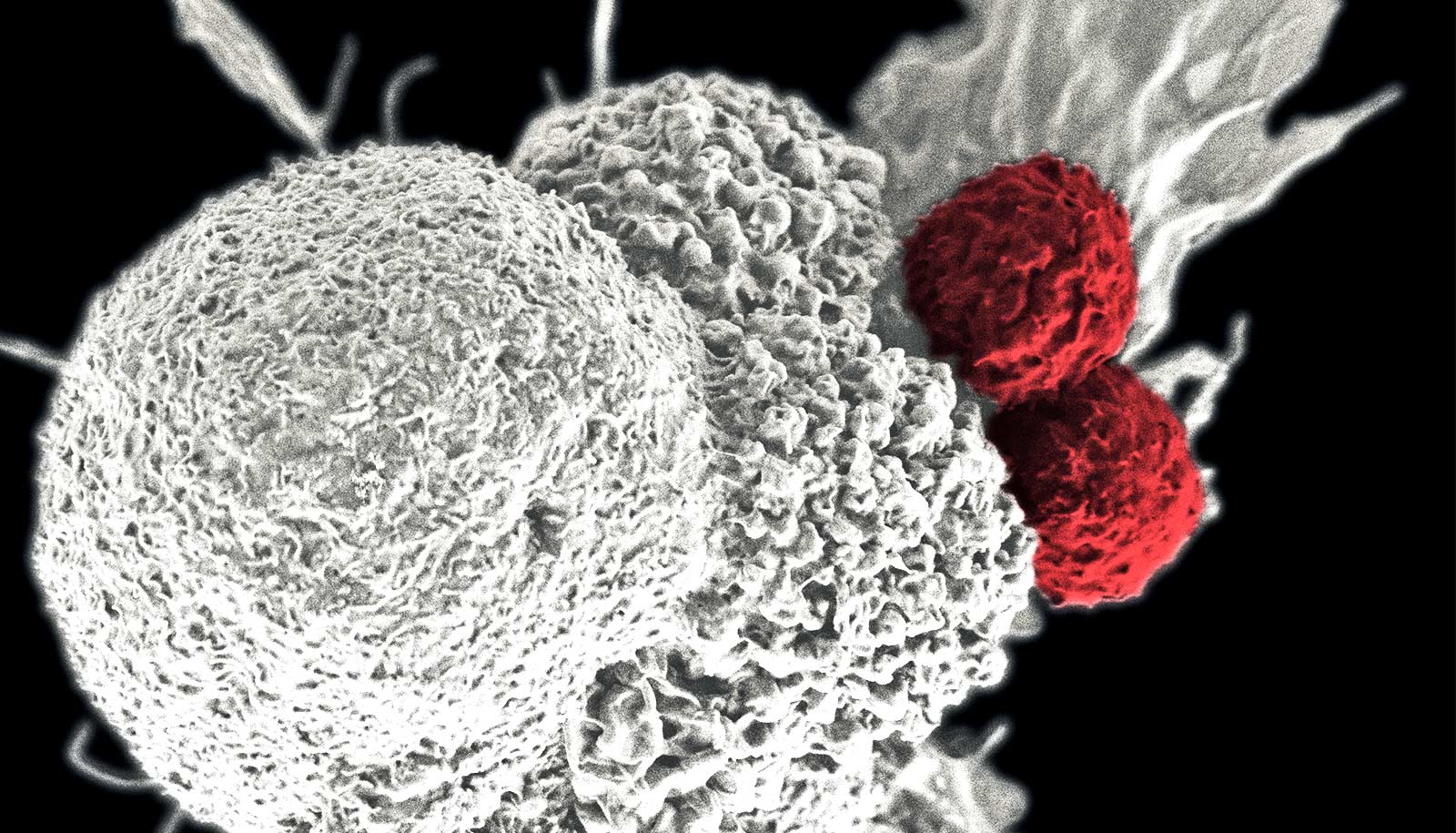
Each neoantigen included in the vaccine raises a red flag for the immune system, sending an army of specialized immune cells called T cells to seek and destroy the tumor.
While the process seems simple in theory, the devil is in the details, and those details reside within the complex inner workings of how cells process and present the neoantigens to the immune system.
For the vaccine to be successful, the neoantigens must be presented to cells in a precise format that maximizes the odds of triggering a complex, step-by-step cascade of natural immune responses. Any misstep may result in a weakened or even failed immune response.
As the new study documents, the neoantigen DNA vaccine can be optimized to improve the presentation process. Small differences in the length of an epitope (the part of the antigen recognized by the immune system), spacing, and amino acid sequence can result in important changes in how neoantigens are presented to the immune system. Even then, cancers often find ways to evade successful attacks.
In this study, Gillanders and his team set out to address these challenges using the latest in next-generation gene sequencing tools, new predictive modeling techniques, and bioinformatics-based computational algorithms—all designed to fine-tune the vaccine creation process.
The findings suggest that longer epitope fragments are more effective at triggering a longer-lasting immune response that includes both CD8 and CD4 T cells; that a mutant marker that tags neoantigens and is cloned to the end of an epitope string can significantly increase its recognition by the immune system; and that even the most well-presented epitopes are seldom successful at shrinking tumors unless accompanied by an additional immunotherapy tool, such as anti-PD-L1 checkpoint blockade.
“Although the initial clinical experience is promising, there is more work to do to refine the vaccines and evaluate their effectiveness in animal models and clinical trials. But this is an important first step and points us in the right direction,” Gillanders says.
Support for the work came from Susan G. Komen for the Cure; the Alvin J. Siteman Cancer Center; the National Institute of Health (NIH); the National Cancer Institute; and the Foundation for Barnes-Jewish Hospital.