A medication used to treat diabetic neuropathy may make chemotherapy treatments more effective for patients with lung cancer, according to a new study.
Despite surgical and chemotherapy treatment, more than 50% of non-metastatic, non-small lung cancer patients see recurrences, in large part because of drug-resistant cancer cells.
Researchers have identified a way to make these cells more susceptible to chemotherapy, says study author Jussuf Kaifi, a thoracic surgeon at the University of Missouri Health Care and an assistant professor of surgery at the university’s School of Medicine.
“Traditional treatments for lung cancer, including chemotherapy, often have little to no effect on the cancer because of drug resistance,” Kaifi says.
“It is a major cause of mortality in patients, so finding ways to circumvent drug and chemotherapy resistance is vital to improving patient outcomes.”
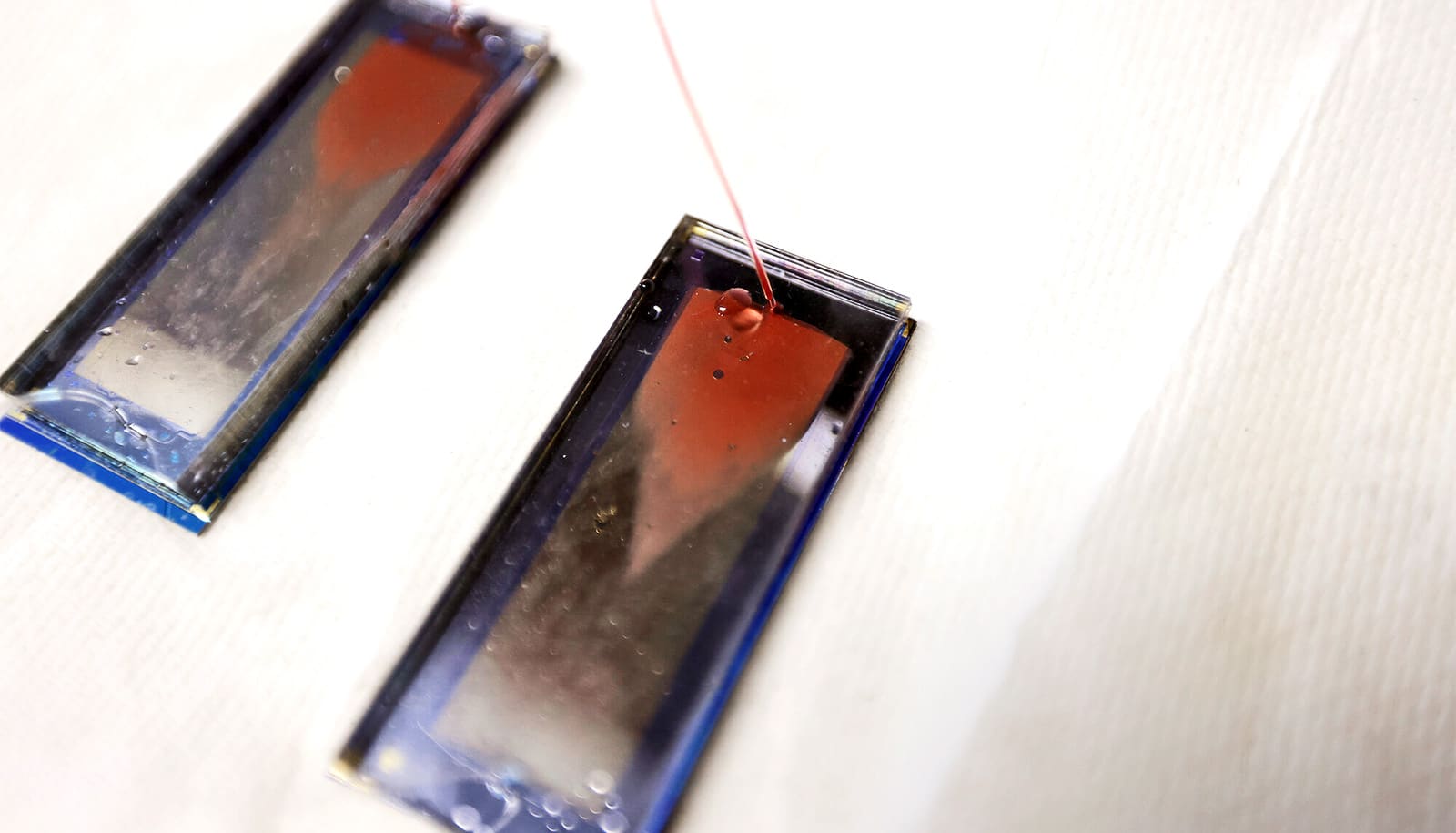
The study examined 10 non-small cell lung cancer tumors, half of which were identified as drug resistant. The drug-resistant tumors showed overexpression of a certain enzyme, AKR1B10. When treated with the diabetic neuropathy medication, epalrestat, the tumors became less drug resistant, causing their sensitivity to chemotherapy to significantly increase.
Epalrestat is available in several countries and well-tolerated by patients, but it is not yet approved for use by the Food and Drug Administration in the United States. The medication is currently in high-level clinical trials as part of the FDA’s approval process. If given FDA approval, epalrestat could be fast-tracked as an anti-cancer drug for lung cancer patients.
“In general, developing new drugs for cancer treatment is an extremely lengthy, expensive and inefficient process,” Kaifi says.
“In contrast, ‘repurposing’ these drugs to other diseases is much faster and cheaper. In view of overcoming drug resistance, epalrestat can rapidly be advanced to the clinic to improve cure rates in lung cancer patients.”
The research appears in Clinical Cancer Research.
Source: University of Missouri