A protein found throughout the body plays a major role in immune system modulation during pregnancy and affects placental health, a study in mice finds.
Immune cells play a key role during pregnancy, adjusting immune system response in a way that enables the fetus to develop while also protecting the parent and fetus from outside assaults like viruses.
The researchers say findings could lead to new treatments for reproductive conditions in the future.
The study, led by Yale School of Medicine’s Reshef Tal, appears in the journal JCI Insight. A human fetus contains genetic material from both parents, which makes it partly foreign to the pregnant person’s body. The immune system, therefore, needs to make adjustments that balance a tolerance for the developing fetus with protection against harmful foreign insults like viruses.
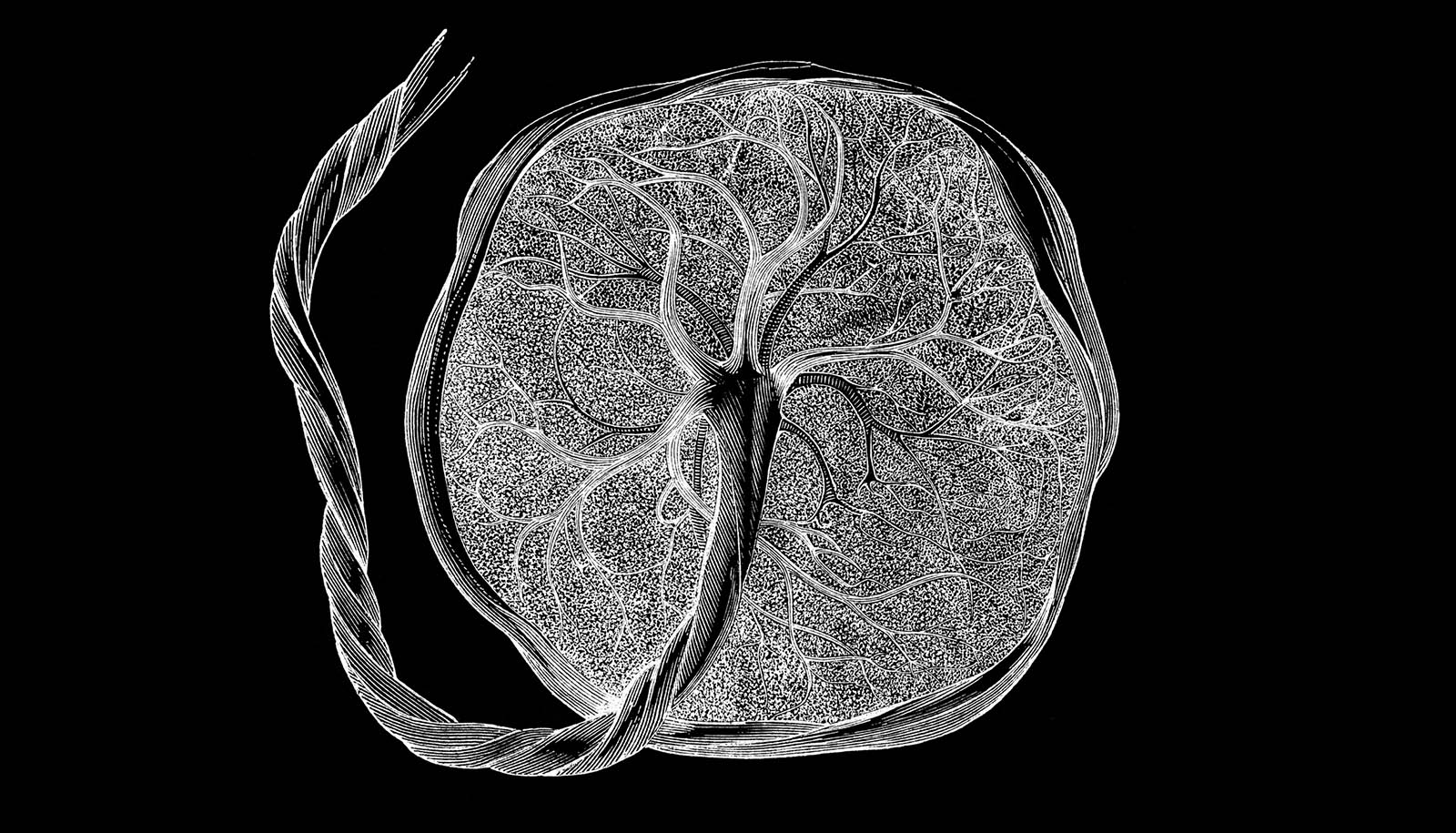
Many of these adaptations happen within the decidua—tissue that surrounds and interfaces with the placenta. Prior studies by the same research team showed that early in pregnancy, bone marrow cells, including immune cells, migrate to the uterus and the decidua. And the researchers were interested in the mechanisms that recruit these cells to the pregnant uterus.
Previous research has shown that a protein called C-X-C chemokine receptor type 4, or CXCR4, and the protein that binds to it are critical for trafficking bone marrow cells in organs and tissues around the body. CXCR4 is also expressed in higher amounts in the uterus at the beginning of pregnancy.
“Previous findings imply there is an important function for CXCR4 in pregnancy,” says Tal, assistant professor of obstetrics, gynecology, and reproductive sciences at Yale School of Medicine and senior author of the study. “We wanted to understand its overall role in pregnancy maintenance and immune function in the decidua.” First, the researchers deleted the gene that codes for CXCR4 in adult female mice, effectively removing the protein from the body. Compared with normal mice, those without CXCR4 lost more fetuses during pregnancy and had smaller litter sizes. However, when CXCR4 was removed only in the uterus, there were no negative pregnancy effects.
“That finding suggested that it’s not the CXCR4 expression within the uterine cells themselves, but rather it’s the CXCR4 expression from outside of the uterus that plays an important role in pregnancy maintenance,” says Tal.
Since immune cells are recruited to the uterus from outside the organ, the researchers then looked at how CXCR4 deletion affected immune cell populations in the decidua. Early in pregnancy, the majority of immune cells in the decidua are what are known as “natural killer” cells. Around the body, these white blood cells destroy diseased cells, but in early pregnancy these natural killer cells in the decidua play a key role in the vast tissue and blood vessel remodeling required for the placenta to properly develop and for the fetus to begin receiving nutrients and oxygen from the parent.
In mice without CXCR4, fewer natural killer cells were trafficked to the uterus and those that were clustered abnormally. These natural killer cells also expressed a particular enzyme (granzyme B) at lower levels than usual, leading to an abnormal inflammatory response in the uterus. Additionally, the mice had irregular blood vessel arrangement in the placenta and decidua, which could affect the exchange of nutrients between parent and fetus.
To see if these changes were caused by immune cell dysfunction, the researchers transplanted healthy bone marrow from normal mice into mice without CXCR4. “We found that this rescued much of the effects,” says Tal.
Mice with transplanted bone marrow had fewer pregnancy losses than those without. They also had normal levels of natural killer cells, cell distribution, expression of enzymes, and blood vessel arrangement in the placenta, the researchers found.
“One of the main takeaways of the study is that you can harness the bone marrow cells’ ability to home to the uterus and affect both the immune status of the decidua and the vascular remodeling of the placenta,” says Tal.
This, he says, could inform new treatments for reproductive conditions like recurrent pregnancy loss and preeclampsia.
“In these conditions, there is thought to be an imbalance in the immune factors and the factors involved in blood vessel formation,” says Tal. “Our findings could potentially lead to a cell therapy approach to treat those types of conditions.”
Source: Yale University