A new test can determine within 10-15 minutes whether patients test positive for COVID and, if so, which of the five known variants of concern they have.
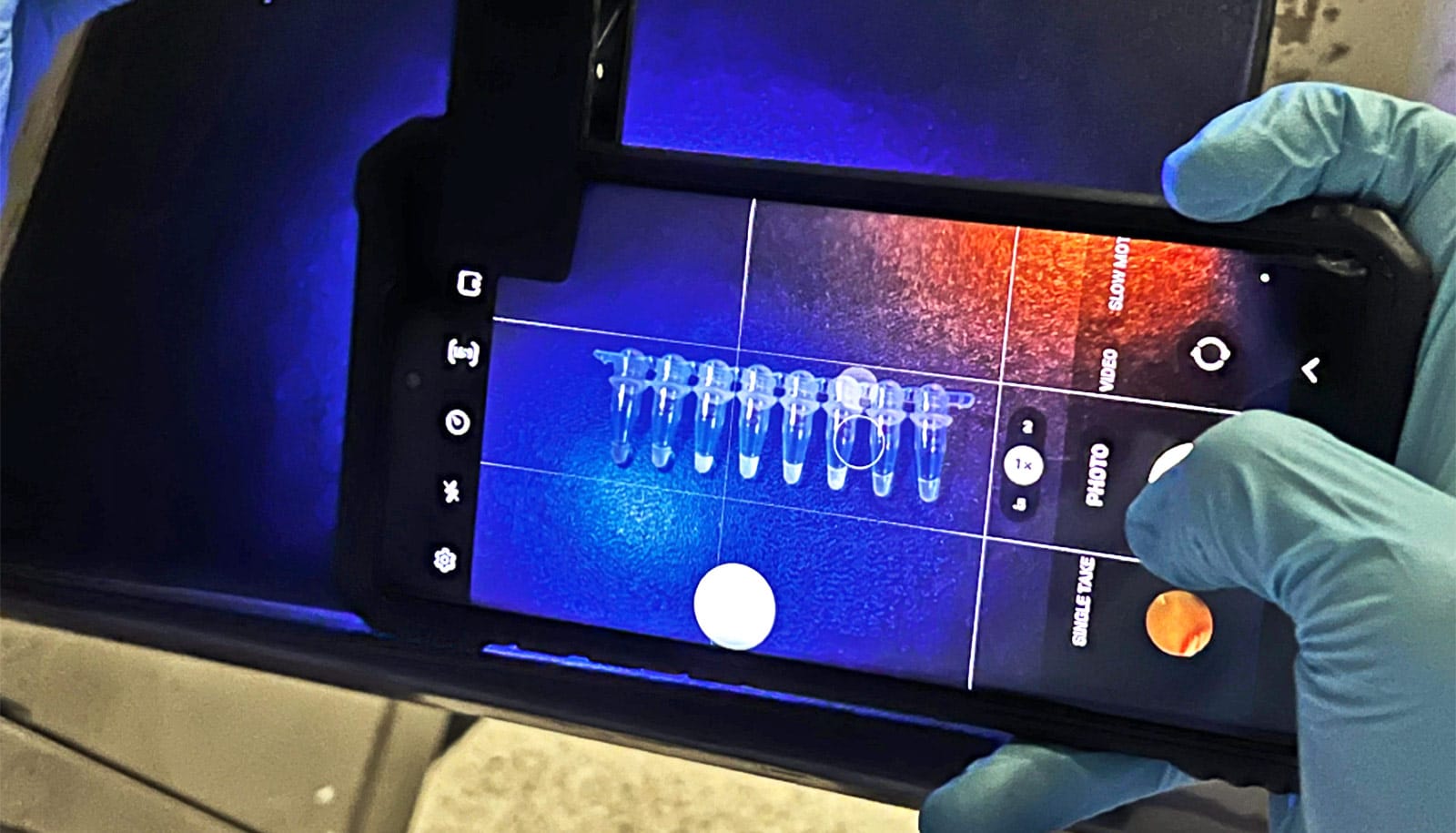
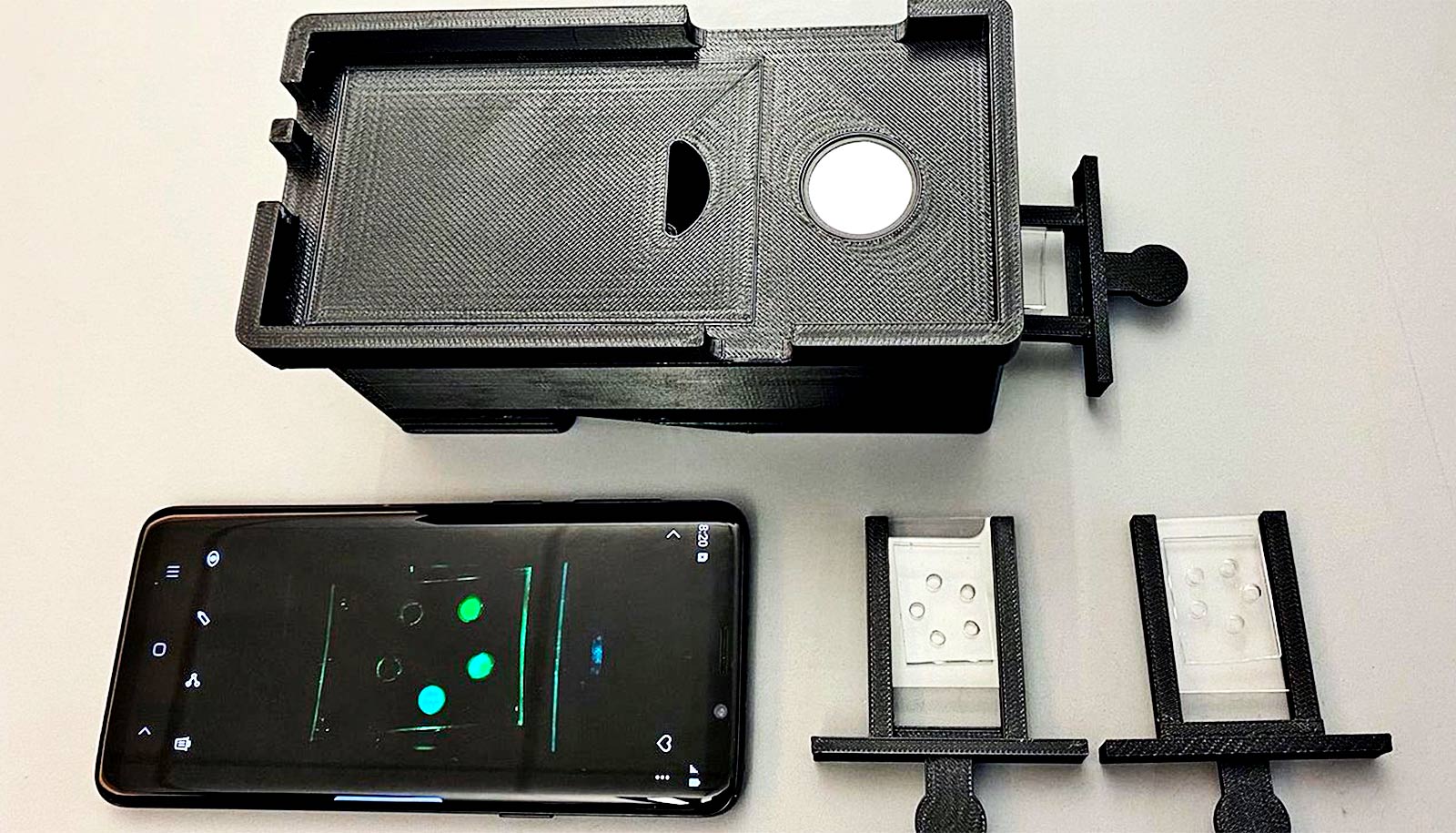
The research involves the use of a simple heating device and a cellphone. The researchers also used a new form of CRISPR—a means of finding and targeting a specific section of genetic material inside a cell—to quickly and effectively diagnose COVID and learn which variant of concern is in a patient sample: Alpha, Beta, Gamma, Delta, or Omicron.
The findings could provide policymakers with vital information about when to require masking and prepare hospitals for a wave of infections. It could also allow patients and family members to prevent or treat a particular variant more effectively.
“For the medical and research community, knowing which variants are emerging is extremely important,” says corresponding author Piyush Jain, an assistant professor in the chemical engineering department at the University of Florida.
“If an especially serious variant like Delta or a genetically similar variant, such as Deltacron, arises in the future, work like this discovery will help us track it earlier.”
Current processes for determining COVID variants take several days to perform, which is why patients typically don’t learn which variant they have.
Advancing on recently published work, including by Long Nguyen, a PhD candidate and the first author of the study, the researchers are the first to investigate the new heat-loving CRISPR technology, which manages to combine speed, accuracy, and variant identification by amplifying and detecting coronavirus genetic material in one step.
The team also created a version of the COVID test that can potentially be used at commercial testing centers, or even at home, and can be stored at normal temperatures for weeks and activated by adding water.
Researchers validated the test in hundreds of clinical samples, detecting all five variants with 97% accuracy within 30 minutes.
Jain, who says he hopes the product can be brought affordably to market soon, worked with Rhoel Dinglasa, a professor of infectious diseases and immunology, and others to establish a startup called Genable Biosciences, LLC, centered around finding partners to manufacture and commercialize the new product.
The study appears in in eBioMedicine.
Source: Catherine Arnold for University of Florida