With flu season right around the corner in the United States, and Omicron subvariants of the coronavirus still circulating, many people are wondering if they should get their influenza vaccine and the latest COVID-19 booster shot together.
“Absolutely. The CDC is recommending that you get your flu shot and your booster shot at the same time,” says infectious disease specialist Sabrina A. Assoumou.
For many, getting both shots at the same time is just plain convenient.
“It’s safe—we know it’s fine to get both at the same time,” says Assoumou, a professor of medicine at Boston University. “And getting both at once means that you don’t have to go back for a second shot, something that may or may not actually happen.”
Here, Assoumou, who is an attending physician in the infectious diseases section at Boston Medical Center, BU’s primary teaching hospital and the city’s safety net hospital, provides answers to other burning questions about COVID-19 vaccines, boosters, and mitigation strategies:
One shot in each arm or both in one arm?
At a press conference this month, Ashish Jha, who leads the White House pandemic response, quipped, “God gave us two arms—one for the flu shot and the other one for the COVID shot.”
“It’s a funny remark,” Assoumou says, “and it’s also good advice. Most people will recommend getting one shot in each arm,” she says, adding that ultimately, it really comes down to personal preference.
Will the side effects be worse if you get both shots at once?
According to the Centers for Disease Control and Prevention (CDC): “Experience with other vaccines has shown that the way our bodies develop protection, known as an immune response, and possible side effects after getting vaccinated are generally the same when given alone or with other vaccines.”
Anecdotally, Assoumou says she opted to get both her booster and flu vaccines at the same time.
“I felt tired, but it was worth it to know that my body was developing immunity that would protect me down the line,” she says.
If you’ve recently had COVID-19, do you need the new booster?
Assoumou says you should still get it, but wait a few months. The CDC recommends waiting three months since your last infection before getting a booster shot. This allows for the most effective immunity from SARS-CoV-2, the virus that causes COVID-19. Assoumou compares receiving vaccination after infection to taking classes: “You don’t want to start a new course before you’re done with the last one.”
Can children and teenagers get the new booster?
So far, the Food and Drug Administration has authorized the Pfizer-BioNTech booster for everyone aged 12 and older, and the Moderna booster for everyone aged 18 and over—but the Biden administration’s vaccine chief, Peter Marks, expects new authorization for younger children soon. Authorization for the country’s youngest children, those five and under, is still likely a few months away.
Once shots are available, Assoumou generally recommends getting one as soon as possible.
“My thoughts are usually that when cases are high, it is best to get your shot as soon as you are eligible, instead of trying to strategize,” she says. “What ends up happening is that one often gets infected while waiting. We anticipate that cases are going to rise in the fall and winter, so it is best to get vaccinated as soon as one is eligible.”
What makes this COVID-19 booster different from previous shots?
The newest booster is known as a bivalent vaccine, which means that it targets different strains of SARS-CoV-2 at the same time, Assoumou says.
One component of the mRNA vaccine targets the Omicron subvariants BA.4 and BA.5, which are currently circulating in the United States. Another component targets the virus’ ancestral strain, or the original strain.
This is new. Previous vaccines and boosters have been monovalent, meaning they only targeted one variant of the virus, Assoumou says.
“Part of the reason this has changed is that we simply have the technology to adapt to new strains faster now,” she says.
Another reason to attack two variants at once? “We don’t know what’s coming around the corner,” Assoumou says. The bivalent vaccine provides targeted protection against the most common strains right now, as well as broad protection from SARS-CoV-2.
Should we expect to keep encountering new strains of the virus?
“Unfortunately, SARS-CoV-2 is here to stay,” Assoumou says. “It’s going to keep evolving, and we’re going to see new variants. BA.5 is what we have now, but it isn’t the last one.”
The good news: we have vaccines.
“Vaccination is how we emerge from this pandemic,” she says. “We have to vaccinate more people in the country; we have to vaccinate the world. That’s ultimately how we prevent these variants from evolving.”
If we’re fully boosted, do we still have to wear masks?
“A lot of us talk about a layered approach to the pandemic,” Assoumou says. “The first layer is vaccination: what’s going to get us to the other side of this is immunity in the community.”
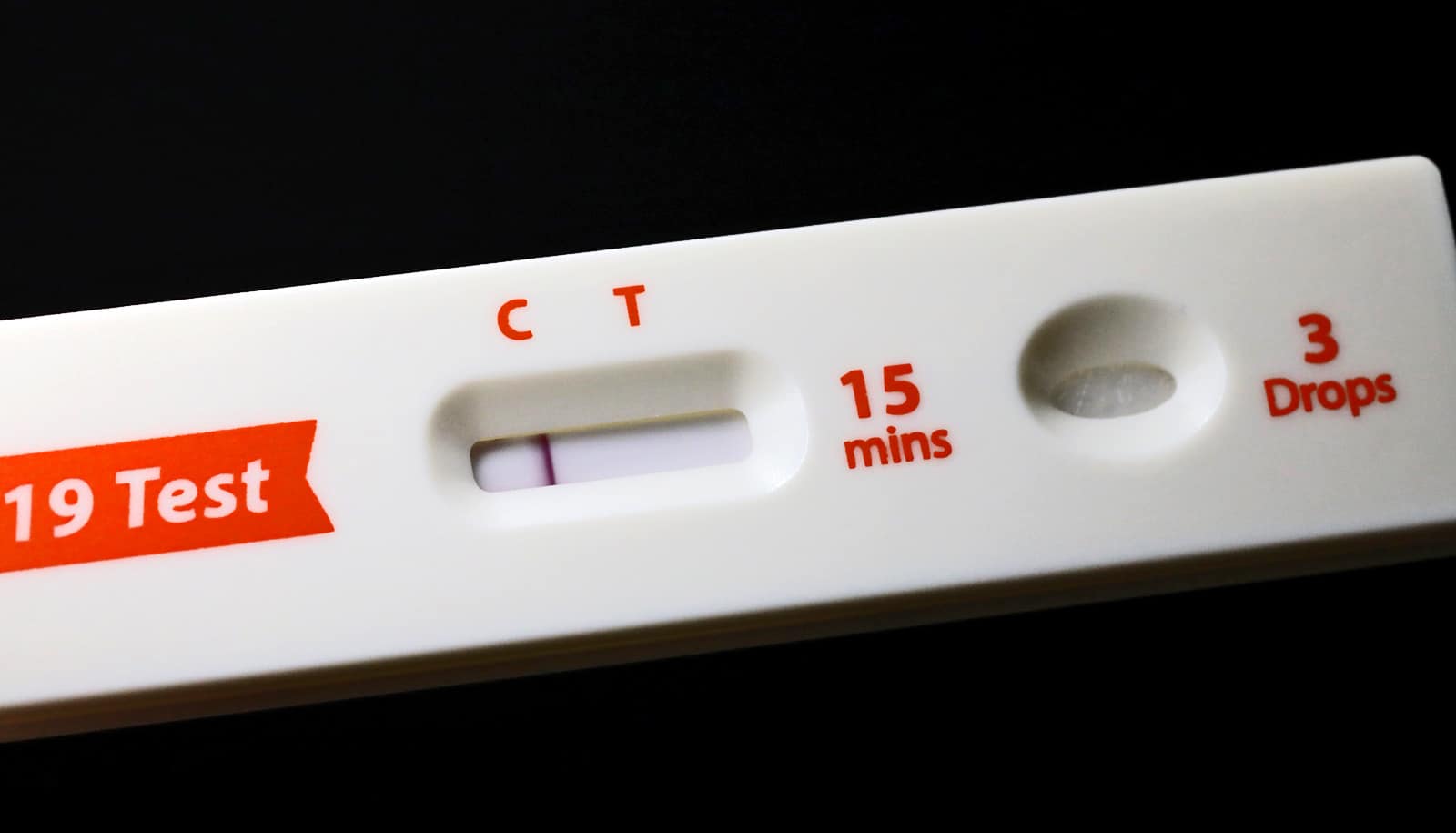
But, she adds, the other layers—including masking, testing, and updating ventilation indoors—are just as important.
“What we’re learning over the past two or three years is that a vaccine-only approach will only get us so far. We also need to mask when we’re in a community where there’s high transmission, improve indoor ventilation, and take advantage of testing if we think we’ve been exposed,” she says.
Think of it like the weather, Assoumou says: if you see rain in the forecast, bring an umbrella. Similarly, keep an eye on the local COVID-19 forecast: if cases are rising around you, bring a mask.
COVID-19 vaccines (and other mitigation efforts) are important. But do you really need a flu shot?
Influenza appears ready to make a big comeback this year.
“Generally, we can use what happens in the Southern Hemisphere as foreshadowing for infection during the winter months here,” Assoumou says. Because the flu season in southern countries typically runs from April to October, a particularly tough winter in Australia and New Zealand—both countries saw their highest rates of influenza in years—spells trouble for the United States, where flu infections peak a few months later, from December to February.
“This is a good year to get vaccinated,” Assoumou says. And because the same mitigation strategies we use for COVID-19 (masking and proper ventilation in particular) also work to keep influenza at bay, the United States has so far avoided a “twindemic” of COVID-19 and flu cases.
“Let’s try to keep it that way,” Assoumou says.
Source: Molly Callahan for Boston University